Classification of meningiomas—advances and controversies
Introduction
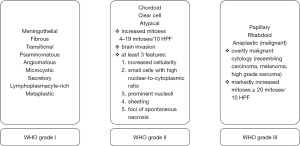
Meningiomas are the most frequent primary tumors of the central nervous system (CNS) (1). Due to their heterogenous morphological features former and the current edition of the World Health Organization (WHO) classification of tumors of the CNS provide 15 distinct meningioma variants (Figure 1). Despite the morphological diversity, patient prognosis is often very good, which is mainly due to the benign, slow growing character of the tumors. Depending on the tumor localization, benign meningiomas are basically tumors that can be cured by neurosurgical resection (2). In line with that the extent of resection, reflected by the Simpson grade is a strong predictor of tumor recurrence (2,3). Nevertheless, in a study by Jääskeläinen up to 20% of benign gross-totally resected meningiomas recurred within 20 years (4). Consequently, a good argument can be made that there are subgroups of meningiomas that tend to recur or even show malignant transformation although gross-total resection was achieved.
An adequate classification system basically aims at providing a tool for estimating the risk of tumor recurrence and estimating the overall survival of a patient. In the best case the classification system should even take into account a prediction towards the response to a certain therapy.
The WHO classification of CNS tumors stratifies meningiomas in three major groups, reflected by the WHO grades I (benign), II (intermediate) and III (malignant) (5) (Figure 1). So far the diagnostic work flow of the current WHO classification for meningiomas strictly relies on histo- and cytomorphological criteria (5). WHO grade and extent of resection are still the most important predictors of progression-free survival (PFS) and should therefore be reported for every individual patient (2). However, for some patients WHO grading seems insufficient as (I) almost 20% of benign WHO grade I tumors tend to recur (4,6,7) and (II) adjuvant radiotherapy might not be necessary for all WHO grade II meningiomas (8-10). The discordance between clinical course and histological grade might depend on the application of histological criteria, which for some reasons are difficult to assess in meningiomas or which do not reflect the entire biological character of the tumor (see especially paragraphs “Tightrope walk between meningioma grades” and “Brain invasion as an individual criterion for atypia”).
In the current review article we discuss the diagnostic criteria for meningiomas as applied by the current WHO classification for CNS tumors (5). We present advances of the classification system as well as some controversies, which might lead to an over- or underestimation of the biological tumor properties. Furthermore we will illustrate the latest mostly genetic discoveries in meningioma research and provide an outlook for future meningioma classifications.
Histo- and cytopathological basis of meningioma classifications
Meningiomas are subdivided in 15 histo- and cytomorphological variants of which nine variants correspond to WHO grade I, three variants correspond to WHO grade II, while another three variants correspond to the malignant type of WHO grade III meningiomas (Figure 1) (5). The majority of meningiomas correspond to WHO Grade I with an age-adjusted incidence rate of 3.68/100,000 in male and 8.56/100,000 in female population (11). The age-adjusted incidence rate in WHO grade II meningiomas accounts for 0.26/100,000 in male and 0.30/100,000 in female population (11). WHO grade III meningiomas are a rare disease with an age-adjusted incidence rate of 0.08/100,000 in male and 0.09/100,000 in female population (11).
The most common histomorphological subtypes are WHO grade I meningothelial, fibrous and transitional meningiomas (5). The histological criteria, applied in the current classification system are mainly based on the groundbreaking work by Perry and colleagues (12,13) who showed that different cyto- and histomorphological features were associated with tumor recurrence. Nevertheless, also earlier important follow-up investigations on meningioma classification influenced the current WHO classification systems (14,15). Finally, this lead to the criteria for considering meningiomas as being atypical (grade II) in case they showed increased mitotic activity [4–19 mitoses per 10 high power fields (HPF)] or at least 3 of 5 histo- and cytomorphological criteria (Figure 1). An alternative grading approach combines hypercellularity and mitotic count for the diagnosis of atypical meningioma (≥5 mitoses per 10 HPF) (15). Furthermore, already in their 1997 study, Perry and colleagues suggested brain invasion as a morphologic criterion for higher recurrence rates (12) (see paragraph “Brain invasion”). Despite their partly benign appearance the distinct histomorphological subtypes of clear cell and chordoid meningiomas are considered WHO grade II, as these tumors tend to recur (16,17).
The basic criteria for grading meningiomas as being malignant or anaplastic also arose from Perry and colleagues in 1999 (13). In their 1999 publication the authors proposed a revision of the histological grading scheme for meningiomas including a definition of atypical and anaplastic meningioma (13). Meningiomas were considered being anaplastic in case the tumors showed 20 or more mitoses/10 HPF or a loss of meningothelial differentiation resulting in sarcoma-, carcinoma- or melanoma-like appearance (13) Rhabdoid and papillary meningiomas were considered malignant as well, as these patients showed a very poor prognosis with multiple recurrences and even distant metastases (18-21).
These cyto- and histopathological criteria contributed to the current WHO classification system (5) (Figure 1) and are still most often successfully applied in routine neuropathological diagnostics for grading meningiomas. Despite of the significance of these criteria still some of the histopathological features need a closer look and a potential revision in future classification systems.
Tightrope walk between meningioma grades
When applying the aforementioned criteria in everyday routine diagnostics one would always meet borderline cases, which make it difficult to draw a clear line between the grades especially between benign (WHO grade I) and intermediate (WHO grade II) cases. Interestingly, patients with WHO grade I tumors and any atypical features (one or two of the aforementioned five) show increased risk for tumor progression or recurrence, when Simpson grade I resection was not achieved (22). Illustrating the importance of documentation of the grade of resection as well as the documentation of single atypical features for patients risk stratification. Additionally, in the same study the authors revealed a Ki67-proliferation index >3% (assessed by MIB1 immunohistochemical staining) as being significantly associated with tumor progression or recurrence (22). The application of a proliferation index for risk stratification in meningioma patients is by far not a new notion (23,24), as already former WHO classifications refer to the importance of the proliferation index when stratifying the risk of meningioma recurrence. Nevertheless, e.g., Ki67 proliferation index was not considered as a clear criterion for atypical or anaplastic meningiomas in former and in the current WHO classification (5,25,26), which is most likely because of potential institutional differences. One further challenge for including Ki67 proliferation index into the classification system would be finding a clear threshold. As mentioned above some authors report on proliferation indices of >3% others of >5% or even >10% being associated with an increased risk of tumor progression or recurrence (2,22,27).
Ki67 is a molecule being expressed in cells that are in the active phase of the cell cycle (G1-, S-, G2-, M-phase). Thus Ki67 is related to cell division. The easiest way of assessing cell division is counting mitoses. The number of mitoses per 10 HPF is one of the fundamental criteria of current and former meningioma grading systems (5,25,26). The analysis of discordance rates in the assessment of mitoses per 10 HPF recently revealed a discordance rate of 20.9% between observers, when classifying between grade I meningioma and atypical grade II meningiomas (4–19 mitoses per 10 HPF) (28). Interestingly, discordance rate was much lower (4.7%) when classifying between grades II and III (>20 mitoses per 10 HPF). That means, malignant meningiomas, which are rich in mitotic figures can be assessed rather easy in comparisons to meningiomas with reduced mitotic activity. Some challenges in the assessment of mitotic figures might be the distinction between mitosis and apoptosis as well as the variability of cell density and other tissue properties such as mineralizations. Therefore, also in the context of detecting dividing cells additional immunohistochemistry might be helpful. One prominent candidate is the mitosis-specific protein phosphohistone-H3 (pHH3) (29). Additional pHH3-immunostaining increases interobserver agreement in mitotic count when grading meningiomas (30).
A mitotic index which includes assessment of mitoses with the help of pHH3-staining is an independent predictor of meningioma recurrence (31).
Institutional/observer concordance of meningioma classification and grading has recently been investigated on the basis of the NRG Oncology RTOG Trial 0539 by a central review (28). Discordance rate between observers with regard to the WHO grade was quite low (WHO grade I: 7%; WHO grade II: 12.2%; WHO grade III: 6.4%), thus, leading to a reclassification of diagnosis in 12.8% of tumors (28). On histological level, e.g., hypercellularity, sheeting and the presence of macronucleoli showed highest discordance rates (28). But also the presence of papillary or rhabdoid tumor parts, which in fact has a crucial impact on prognosis and therapy was not always concordant between the observers, thus showed lower interrater reliability values (28). Recently, a study revealed that meningiomas with rhabdoid features showed recurrence rates comparable to grade I and II meningiomas, while just a subset of rhabdoid meningiomas showed an aggressive behavior. In consequence of these findings the authors recommended to classify rhabdoid meningiomas according to grade I and II but with the addition, that aggressive behavior might occur (32). In case of just focal rhabdoid morphology and missing histological signs of malignancy, these tumors should be graded according to the aforementioned classical cyto- and histopathological criteria with the added descriptor of “with rhabdoid features”. The morphologically malignant phenotypes should be classified according to WHO grade III (5).
Brain invasion as an individual criterion for atypia
Interestingly, the assessment of brain invasion showed highest concordance levels of all investigated histopathological features in the aforementioned centrally reviewed NRG Oncology RTOG Trial 0539 (28). While histopathological signs of atypia such as sheeting, high cellularity, macronucleoli, small cells or necrosis are commonly accepted as criteria for atypia, brain invasion as single criterion has recently been questioned. Several studies lacked a clear association between brain invasion and tumor recurrence/progression (27,33-35). The 2016 edition of the WHO classification for CNS tumors now included brain invasion as a single criterion for grading these tumors directly as atypical meningiomas (5). Consequently, patients that show a histologically benign (WHO grade I) but brain invasive meningioma (brain invasive otherwise benign) need a closer look. Pioneering studies concerning with the topic of brain invasion just included 10 (12) or 20 (13) brain invasive otherwise benign meningiomas. Nevertheless, the authors here identified a clinical course similar to atypical meningiomas. Recent studies investigated 61 (27), 19 (33) or 20 (35) patients with brain invasive otherwise benign meningiomas at four independent Brain Tumor Centers in Europe. Most of these investigated patients showed a clinical course similar to WHO grade I meningiomas, with the exception of single patients that showed e.g., an increased proliferation rate, NF2 germline mutation or incomplete resection (Simpson grade 4) (27). The assessment of brain-invasive areas strongly correlates with tumor size, and the number of sampled blocks (27,33). Obviously, most of the tumor parts of meningiomas are not directly attached to the brain surface, thus a critical evaluation of these tumor parts with regard to brain invasion is impossible. Therefore, an adequate assessment of brain invasion would need a close collaboration between the neurosurgeon and the neuropathologist, which could just be guaranteed by setting clear standards for the processing and assessment of meningiomas. So far the WHO does not clearly recommend such a procedure.
Morphology and anatomy meet genetics
Already former editions of the WHO classification of CNS tumors point to the importance of genetic alterations during meningioma progression, since histologically benign meningiomas do not show genetic changes as their high-grade counterparts (36-38). One cytogenetic alteration of meningiomas is the monosomy of Chromosome 22 (39). Chromosome 22 harbors the tumor suppressive NF2 gene locus, being mutated in more than 50% of sporadic and neurofibromatosis type 2 associated meningiomas (40,41). NF2 mutations or NF2 loss mainly leads to a non-functional merlin protein, which in turn most likely serves as an early and main inducer of NF2-associated meningiomas (42). NF2 inactivation results in chromosomal instability (43) and is more often associated with atypia (44). Besides NF2, also other genes on Chromosome 22 such as INI1 (SMARCB1) have been found being mutated in meningiomas, which might contribute to meningioma genesis (45).
Interestingly, NF2 mutated meningiomas show an association with localization (convexity) and histopathological subtype (transitional and fibroblastic) (46). The association of tumor localisation and/or histopathological phenotype, with a distinct genotype has recently been investigated in depth (44,47-49). These findings mainly affect NF2-wildtype, benign WHO grade I meningiomas at the skull base. Anterior and medial skull base meningiomas are NF2-wildtype, while lateral and posterior meningiomas are associated with NF2 loss (44). Medial anterior skull base meningiomas more often show SMO mutations (Hedgehog signaling), while AKT1 (AKT-PI3K signaling) mutation is found in meningothelial and transitional meningiomas of the sella and clivus (44,47,50). Interestingly, recent work investigated SMO and AKT1 mutations in olfactory groove meningiomas. WHO grade I meningiomas with SMO mutations were associated with a reduced time to progression. Thus, this study identifies SMO mutations as a prognostic marker in olfactory groove meningiomas (51). Recently, PIK3CA-mutated meningiomas have also been discovered. Most of these tumors are WHO grade I meningiomas arising from the skull base (52). Secretory meningiomas are genetically characterized by TRAF7 and KLF4 mutations, these mutations occur in combination in almost 100% of these cases (44,48). Recently, another genetic subset of meningiomas has been discovered, when focusing on meningiomas, which lacked the aforementioned mutations. In a genetic screening POLR2A mutations were detected in benign histologically meningothelial meningiomas, which showed a tendency to develop from the tuberculum sellae (49). Interestingly, the same study revealed NF2 and SMARCB1 mutated meningiomas, which originated from the falx cerebri of the anterior cavity. Furthermore, PI3K pathway mutations were detected in TRAF7 mutated meningiomas (49).
Although, these reclassifications of histologically characterized meningiomas by means of gene alterations might somehow give the impression of excessive descriptive anatomical genetics, these studies are urgently needed for uncovering predictive molecular factors and molecular targets.
The last years were characterized by enormous progress on genetic understanding of meningioma genesis especially of benign meningiomas. But also former and recent investigations have been performed to get new insights in the progression of meningiomas. Mainly chromosomal aberrations, such as aberrations of chromosomes 1p and 14q have been described as being associated with higher-grade meningiomas and reduced PFS (53-56). Further cytogenetic investigations on chromosomal abnormalities (losses, gains) identified chromosome 14 abnormalities as being independent adverse prognostic factors in meningiomas (57). Additionally, alterations of the tumor suppressor gene CDKN2A (p16) and deletions of the chromosomal region 9p21 have been linked to anaplastic meningiomas and worse patient prognosis (58-60). Besides inactivation of tumor suppressors also overexpression of telomerase by TERT promoter mutations has been shown to be crucial for malignant progression in both, NF2-mutated (NF2-loss) as well as in NF2-wildtype meningiomas (61,62). Most interestingly, the analysis of TERT-promoter mutation is a strong prognosticator for meningioma patients’ risk stratification and is associated with rapid recurrence also in case of otherwise benign histology (62).
Conclusions and outlook
Up to now, meningioma classification by the WHO strictly relies on histopathological criteria. In many cases these cyto- and histopathological features help to estimate patient prognosis. Nevertheless, still some patients are misgraded, most likely due to limitations of the applied histopathological criteria. As an example the grading of brain invasive otherwise benign meningiomas as atypical (WHO grade II) should be revised in the next edition of the WHO classification as these tumors usually show clinical courses similar to WHO grade I. Additionally, meningiomas with rhabdoid features should not directly be graded as grade III as just a subset show malignant progression. In case of focal rhabdoid features but otherwise benign or atypical histology (not anaplastic), a descriptor of “with rhabdoid features” should be added. Further genetic testing is recommended for these rare cases. For risk stratification a genetic profile including genes which are most often associated with benign tumors (such as TRAF7, AKT1, KLF4, SMO, PIK3CA and POLR2A) and the assessment of alterations which are associated with malignant progression such as TERT-promoter mutation should be included to an integrated histopathological and molecular diagnosis.
A global classification system as desired by the WHO should be applicable in every neuropathological or pathological department worldwide, also in areas where high-throughput genetic screenings are not accessible in everyday routine. One possibility would be the assessment of immunohistochemical surrogate parameters, such as SFRP1 or STMN1 expression in AKT1 (E17K)-mutated meningiomas or GAB1 and STMN1 expression in SMO mutated meningiomas (47,50). Valuable diagnosis and therapy of meningioma patients need a multidisciplinary approach, which ideally should include information on macroscopy (Simpson grade), microscopy (histological parameters) and genetic changes.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Ostrom QT, Gittleman H, Fulop J, et al. CBTRUS Statistical Report: Primary Brain and Central Nervous System Tumors Diagnosed in the United States in 2008-2012. Neuro Oncol 2015;17 Suppl 4:iv1-iv62. [Crossref] [PubMed]
- Gousias K, Schramm J, Simon M. The Simpson grading revisited: aggressive surgery and its place in modern meningioma management. J Neurosurg 2016;125:551-60. [Crossref] [PubMed]
- Simpson D. The recurrence of intracranial meningiomas after surgical treatment. J Neurol Neurosurg Psychiatry 1957;20:22-39. [Crossref] [PubMed]
- Jääskeläinen J. Seemingly complete removal of histologically benign intracranial meningioma: late recurrence rate and factors predicting recurrence in 657 patients. A multivariate analysis. Surg Neurol 1986;26:461-9. [Crossref] [PubMed]
- Louis DN, Perry A, Reifenberger G, et al. The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary. Acta Neuropathol 2016;131:803-20. [Crossref] [PubMed]
- van Alkemade H, de Leau M, Dieleman EM, et al. Impaired survival and long-term neurological problems in benign meningioma. Neuro Oncol 2012;14:658-66. [Crossref] [PubMed]
- Gallagher MJ, Jenkinson MD, Brodbelt AR, et al. WHO grade 1 meningioma recurrence: Are location and Simpson grade still relevant? Clin Neurol Neurosurg 2016;141:117-21. [Crossref] [PubMed]
- Rogers L, Gilbert M, Vogelbaum MA. Intracranial meningiomas of atypical (WHO grade II) histology. J Neurooncol 2010;99:393-405. [Crossref] [PubMed]
- Lagman C, Bhatt NS, Lee SJ, et al. Adjuvant Radiosurgery Versus Serial Surveillance Following Subtotal Resection of Atypical Meningioma: A Systematic Analysis. World Neurosurg 2017;98:339-46. [Crossref] [PubMed]
- Talacchi A, Muggiolu F, De Carlo A, et al. Recurrent Atypical Meningiomas: Combining Surgery and Radiosurgery in One Effective Multimodal Treatment. World Neurosurg 2016;87:565-72. [Crossref] [PubMed]
- Kshettry VR, Ostrom QT, Kruchko C, et al. Descriptive epidemiology of World Health Organization grades II and III intracranial meningiomas in the United States. Neuro Oncol 2015;17:1166-73. [Crossref] [PubMed]
- Perry A, Stafford SL, Scheithauer BW, et al. Meningioma grading: an analysis of histologic parameters. Am J Surg Pathol 1997;21:1455-65. [Crossref] [PubMed]
- Perry A, Scheithauer BW, Stafford SL, et al. “Malignancy” in meningiomas: a clinicopathologic study of 116 patients, with grading implications. Cancer 1999;85:2046-56. [PubMed]
- Kallio M, Sankila R, Hakulinen T, et al. Factors affecting operative and excess long-term mortality in 935 patients with intracranial meningioma. Neurosurgery 1992;31:2-12. [Crossref] [PubMed]
- Maier H, Ofner D, Hittmair A, et al. Classic, atypical, and anaplastic meningioma: three histopathological subtypes of clinical relevance. J Neurosurg 1992;77:616-23. [Crossref] [PubMed]
- Zorludemir S, Scheithauer BW, Hirose T, et al. Clear cell meningioma. A clinicopathologic study of a potentially aggressive variant of meningioma. Am J Surg Pathol 1995;19:493-505. [Crossref] [PubMed]
- Couce ME, Aker FV, Scheithauer BW. Chordoid meningioma: a clinicopathologic study of 42 cases. Am J Surg Pathol 2000;24:899-905. [Crossref] [PubMed]
- Ludwin SK, Rubinstein LJ, Russell DS. Papillary meningioma: a malignant variant of meningioma. Cancer 1975;36:1363-73. [Crossref] [PubMed]
- Pasquier B, Gasnier F, Pasquier D, et al. Papillary meningioma. Clinicopathologic study of seven cases and review of the literature. Cancer 1986;58:299-305. [Crossref] [PubMed]
- Perry A, Scheithauer BW, Stafford SL, et al. “Rhabdoid” meningioma: an aggressive variant. Am J Surg Pathol 1998;22:1482-90. [Crossref] [PubMed]
- Kepes JJ, Moral LA, Wilkinson SB, et al. Rhabdoid transformation of tumor cells in meningiomas: a histologic indication of increased proliferative activity: report of four cases. Am J Surg Pathol 1998;22:231-8. [Crossref] [PubMed]
- Marciscano AE, Stemmer-Rachamimov AO, Niemierko A, et al. Benign meningiomas (WHO Grade I) with atypical histological features: correlation of histopathological features with clinical outcomes. J Neurosurg 2016;124:106-14. [Crossref] [PubMed]
- Plate KH, Dauch W, Bel S, et al. Zentralbl Neurochir 1990;51:57-68. [Prognosis in meningiomas. Relevance of morphologic studies and clinical risk factors]. [PubMed]
- Ohta M, Iwaki T, Kitamoto T, et al. MIB1 staining index and scoring of histologic features in meningioma. Indicators for the prediction of biologic potential and postoperative management. Cancer 1994;74:3176-89. [Crossref] [PubMed]
- Kleihues P, Louis DN, Scheithauer BW, et al. The WHO classification of tumors of the nervous system. J Neuropathol Exp Neurol 2002;61:215-25; discussion 226-9. [Crossref] [PubMed]
- Louis DN, Ohgaki H, Wiestler OD, et al. The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol 2007;114:97-109. [Crossref] [PubMed]
- Baumgarten P, Gessler F, Schittenhelm J, et al. Brain invasion in otherwise benign meningiomas does not predict tumor recurrence. Acta Neuropathol 2016;132:479-81. [Crossref] [PubMed]
- Rogers CL, Perry A, Pugh S, et al. Pathology concordance levels for meningioma classification and grading in NRG Oncology RTOG Trial 0539. Neuro Oncol 2016;18:565-74. [Crossref] [PubMed]
- Ribalta T, McCutcheon IE, Aldape KD, et al. The mitosis-specific antibody anti-phosphohistone-H3 (PHH3) facilitates rapid reliable grading of meningiomas according to WHO 2000 criteria. Am J Surg Pathol 2004;28:1532-6. [Crossref] [PubMed]
- Duregon E, Cassenti A, Pittaro A, et al. Better see to better agree: phosphohistone H3 increases interobserver agreement in mitotic count for meningioma grading and imposes new specific thresholds. Neuro Oncol 2015;17:663-9. [Crossref] [PubMed]
- Olar A, Wani KM, Sulman EP, et al. Mitotic Index is an Independent Predictor of Recurrence-Free Survival in Meningioma. Brain Pathol 2015;25:266-75. [Crossref] [PubMed]
- Vaubel RA, Chen SG, Raleigh DR, et al. Meningiomas With Rhabdoid Features Lacking Other Histologic Features of Malignancy: A Study of 44 Cases and Review of the Literature. J Neuropathol Exp Neurol 2016;75:44-52. [Crossref] [PubMed]
- Pizem J, Velnar T, Prestor B, et al. Brain invasion assessability in meningiomas is related to meningioma size and grade, and can be improved by extensive sampling of the surgically removed meningioma specimen. Clin Neuropathol 2014;33:354-63. [Crossref] [PubMed]
- Klinger DR, Flores BC, Lewis JJ, et al. Atypical Meningiomas: Recurrence, Reoperation, and Radiotherapy. World Neurosurg 2015;84:839-45. [Crossref] [PubMed]
- Spille DC, Heß K, Sauerland C, et al. Brain Invasion in Meningiomas: Incidence and Correlations with Clinical Variables and Prognosis. World Neurosurg 2016;93:346-54. [Crossref] [PubMed]
- Rempel SA, Schwechheimer K, Davis RL, et al. Loss of heterozygosity for loci on chromosome 10 is associated with morphologically malignant meningioma progression. Cancer Res 1993;53:2386-92. [PubMed]
- Simon M, von Deimling A, Larson JJ, et al. Allelic losses on chromosomes 14, 10, and 1 in atypical and malignant meningiomas: a genetic model of meningioma progression. Cancer Res 1995;55:4696-701. [PubMed]
- Weber RG, Boström J, Wolter M, et al. Analysis of genomic alterations in benign, atypical, and anaplastic meningiomas: toward a genetic model of meningioma progression. Proc Natl Acad Sci U S A 1997;94:14719-24. [Crossref] [PubMed]
- Zang KD. Meningioma: a cytogenetic model of a complex benign human tumor, including data on 394 karyotyped cases. Cytogenet Cell Genet 2001;93:207-20. [Crossref] [PubMed]
- Lekanne Deprez RH, Bianchi AB, Groen NA, et al. Frequent NF2 gene transcript mutations in sporadic meningiomas and vestibular schwannomas. Am J Hum Genet 1994;54:1022-9. [PubMed]
- Wellenreuther R, Kraus JA, Lenartz D, et al. Analysis of the neurofibromatosis 2 gene reveals molecular variants of meningioma. Am J Pathol 1995;146:827-32. [PubMed]
- Kalamarides M, Niwa-Kawakita M, Leblois H, et al. Nf2 gene inactivation in arachnoidal cells is rate-limiting for meningioma development in the mouse. Genes Dev 2002;16:1060-5. [Crossref] [PubMed]
- van Tilborg AA, Al Allak B, Velthuizen SC, et al. Chromosomal instability in meningiomas. J Neuropathol Exp Neurol 2005;64:312-22. [Crossref] [PubMed]
- Clark VE, Erson-Omay EZ, Serin A, et al. Genomic analysis of non-NF2 meningiomas reveals mutations in TRAF7, KLF4, AKT1, and SMO. Science 2013;339:1077-80. [Crossref] [PubMed]
- Schmitz U, Mueller W, Weber M, et al. INI1 mutations in meningiomas at a potential hotspot in exon 9. Br J Cancer 2001;84:199-201. [Crossref] [PubMed]
- Kros J, de Greve K, van Tilborg A, et al. NF2 status of meningiomas is associated with tumour localization and histology. J Pathol 2001;194:367-72. [Crossref] [PubMed]
- Brastianos PK, Horowitz PM, Santagata S, et al. Genomic sequencing of meningiomas identifies oncogenic SMO and AKT1 mutations. Nat Genet 2013;45:285-9. [Crossref] [PubMed]
- Reuss DE, Piro RM, Jones DT, et al. Secretory meningiomas are defined by combined KLF4 K409Q and TRAF7 mutations. Acta Neuropathol 2013;125:351-8. [Crossref] [PubMed]
- Clark VE, Harmancı AS, Bai H, et al. Recurrent somatic mutations in POLR2A define a distinct subset of meningiomas. Nat Genet 2016;48:1253-9. [Crossref] [PubMed]
- Sahm F, Bissel J, Koelsche C, et al. AKT1E17K mutations cluster with meningothelial and transitional meningiomas and can be detected by SFRP1 immunohistochemistry. Acta Neuropathol 2013;126:757-62. [Crossref] [PubMed]
- Boetto J, Bielle F, Sanson M, et al. SMO mutation status defines a distinct and frequent molecular subgroup in olfactory groove meningiomas. Neuro Oncol 2017;19:345-51. [PubMed]
- Abedalthagafi M, Bi WL, Aizer AA, et al. Oncogenic PI3K mutations are as common as AKT1 and SMO mutations in meningioma. Neuro Oncol 2016;18:649-55. [Crossref] [PubMed]
- Sulman EP, Dumanski JP, White PS, et al. Identification of a consistent region of allelic loss on 1p32 in meningiomas: correlation with increased morbidity. Cancer Res 1998;58:3226-30. [PubMed]
- Tabernero MD, Espinosa AB, Maíllo A, et al. Characterization of chromosome 14 abnormalities by interphase in situ hybridization and comparative genomic hybridization in 124 meningiomas: correlation with clinical, histopathologic, and prognostic features. Am J Clin Pathol 2005;123:744-51. [Crossref] [PubMed]
- Jansen M, Mohapatra G, Betensky RA, et al. Gain of chromosome arm 1q in atypical meningioma correlates with shorter progression-free survival. Neuropathol Appl Neurobiol 2012;38:213-9. [Crossref] [PubMed]
- Linsler S, Kraemer D, Driess C, et al. Molecular biological determinations of meningioma progression and recurrence. PLoS One 2014;9:e94987. [Crossref] [PubMed]
- Maillo A, Orfao A, Sayagues JM, et al. New classification scheme for the prognostic stratification of meningioma on the basis of chromosome 14 abnormalities, patient age, and tumor histopathology. J Clin Oncol 2003;21:3285-95. [Crossref] [PubMed]
- Boström J, Meyer-Puttlitz B, Wolter M, et al. Alterations of the tumor suppressor genes CDKN2A (p16(INK4a)), p14(ARF), CDKN2B (p15(INK4b)), and CDKN2C (p18(INK4c)) in atypical and anaplastic meningiomas. Am J Pathol 2001;159:661-9. [Crossref] [PubMed]
- Simon M, Park TW, Köster G, et al. Alterations of INK4a(p16-p14ARF)/INK4b(p15) expression and telomerase activation in meningioma progression. J Neurooncol 2001;55:149-58. [Crossref] [PubMed]
- Perry A, Banerjee R, Lohse CM, et al. A role for chromosome 9p21 deletions in the malignant progression of meningiomas and the prognosis of anaplastic meningiomas. Brain Pathol 2002;12:183-90. [PubMed]
- Goutagny S, Nault JC, Mallet M, et al. High incidence of activating TERT promoter mutations in meningiomas undergoing malignant progression. Brain Pathol 2014;24:184-9. [Crossref] [PubMed]
- Sahm F, Schrimpf D, Olar A, et al. TERT Promoter Mutations and Risk of Recurrence in Meningioma. J Natl Cancer Inst 2015;108:djv377. [Crossref] [PubMed]