The role of Advanced Practice Providers in interdisciplinary oncology care in the United States
Introduction
Advanced Practice Registered Nurses (APRNs) and Physicians Assistants (PAs) are essential to interdisciplinary care of oncology patients. Generally titled in the United States as Advanced Practice Providers (APPs), APRNs and PAs have continued to develop their practice patterns and enhance their roles in oncology care. With the ongoing health care reform, projected increase in cancer incidence (1), and predicted shortage of oncology physicians (2), APPs are increasingly valuable to interdisciplinary oncology care. According to the results of a study commissioned by the American Society for Clinical Oncology (ASCO) in 2007, the demand for oncology visits is expected to increase 48% by 2020 while the supply of oncologists will rise by 14% (3). As projected demand outpaces anticipated resources, the ASCO Workforce Advisory Group recommends improved integration of APPs into the oncology workforce (3).
The majority of APRNs are Nurse Practitioners (NPs) and the American Association of Nurse Practitioners (AANP) reports that there are over 205,000 NPs in the United States in 2015 with 1.2% of these NPs practicing in clinical oncology (4). Other APRNs in oncology include Certified Registered Nurse Anesthetists (CRNAs) and clinical nurse specialists (CNS). Meanwhile, the National Commission on Certification of Physician Assistants (NCCPA) reported 108,717 certified PAs in the United States in 2015 (5). Ross et al. (6) reported that approximately 2.4% of the 75,000 PAs in the United States in 2010 designated oncology as an area of clinical practice.
The APP scope of practice allows for significant contributions across the different stages of the cancer disease trajectory and APPs provide screening and prevention services, diagnosis and treatment, survivorship and surveillance, as well as end-of-life care (3,7-10). APPs can also be found in a variety of community, acute care, and tertiary practice settings in different oncology specialties. Research has documented that oncologists working in teams with APRNs and PAs report improved efficiency, patient care satisfaction, and higher professional satisfaction (3). In the United States, there are states that allow NPs full practice authority without requirement of a signed practice agreement with a collaborating physician (11); however in the oncology specialty, APPs including NPs and PAs are part of an interdisciplinary team that develops plans for active cancer treatment with active engagement and direction of surgical oncologists, medical oncologists and radiation oncologists.
APP education and training vary according to professional track. In order to practice as an APP, one must successfully complete education, training, and then pass a national certification examination as a PA or APRN. Physician Assistant education and training is graduate level education in advanced anatomy, physiology, pharmacology, physical diagnosis, pathophysiology, microbiology, clinical and laboratory science, behavior science, and medical ethics (12) that culminates in entry level practice with a master’s degree. Education and training includes rotations in family medicine, internal medicine, obstetrics and gynecology, pediatrics, general surgery, emergency medicine, and psychiatry (12). All PA students complete these core courses and training components along with electives in their area of interest. Most PA programs are three academic years in length and culminate in a master’s degree (12). The education and training qualifies one for completion of a national certification examination necessary for entry level PA practice. There are also post graduate oncology fellowships for PAs in comprehensive cancer centers that allow for advanced specialization PA oncology practice. At MD Anderson Cancer Center, the one-year PA Fellowship program involves intensive training and instruction under senior oncology clinical PAs and PA educators in various hematology, oncology and solid tumor specialties.
For APRNs, the education and training is determined by the specialty that the APRN decides to pursue at the outset of his or her graduate level education. The most frequently encountered APRNs in oncology are NPs. NPs are Registered Nurses (RNs) who have completed additional graduate education and training to practice with an increased degree of autonomy in assessing health and medical problems as well as with prescribing and evaluating interventions. While the current entry level for NP practice is a Master of Science in Nursing (MSN) degree, the American Association of Colleges of Nursing (AACN) has recommended a shift in preparing NPs with a doctorate in order to enter practice with a Doctor of Nursing Practice or DNP degree (13). The length of a master’s level NP program can range from 15–24 months (14) depending on the specialty focus and the NP student’s part-time or full-time status. NP education comprises of advanced theoretical and clinical instruction on clinical subjects similar as those comprising the PA curriculum but NPs receive instruction emphasizing the development of clinical and professional expertise in a specialty area that the NP student decides to pursue at the outset of his or her program of study. The curriculum prepares the graduate to successfully complete the national certification in their chosen, anticipated area and population of specialty practice (13). The different NP specialty population foci include family health (individual across lifespan), neonatal, pediatrics, adult, gerontology, women’s health, and mental health (14). Additional specialties such as oncology and acute care are also available for NPs (15).
The NP curriculum, regardless of population or specialty focus, incorporates training in competencies that develop scientific foundation, leadership, quality improvement competencies, practice inquiry skills, technology and information literacy, policy competencies, health delivery system competencies, ethics competencies, and independent practice competencies (16). These are designed to equip NPs with core competencies in health care quality improvement, informatics, and evidence-based practice so they can successfully function not only as advanced clinicians but also as valuable contributors and leaders of health care improvement initiatives.
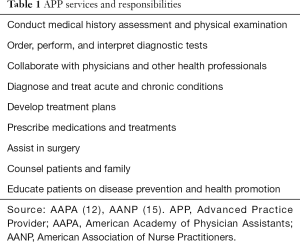
Once in practice, APPs are licensed to diagnose and treat diseases as well manage symptoms. APPs are also licensed with prescriptive authority and can prescribe medications as part of their clinical duties. Table 1 summarizes the services and responsibilities of APPs. Services provided by APPs in oncology were evaluated by the ASCO Study of Collaborative Practice Arrangements (SCPA) in a survey of 266 oncology practices, out of which 33 were selected based on practice size, structure, and geographic distribution (3). The results from the investigation of the study group revealed that APP services included performing clinical procedures, managing disease and treatment, and providing education and counseling. Duties such as chemotherapy orders, inpatient rounds, research-related activities, symptom management, survivorship care, end-of-life care, and providing non-cancer related primary care were also specified in the report. The various activities generally fall into clinical, education, research, and administrative categories. As the health care system continues to evolve, APPs are called upon in their various areas of oncology practice to optimize the integration of these responsibilities to help improve patient care outcomes.
Full table
Screening & prevention programs
APPs provide many cancer screening and prevention services in collaboration with physicians, and the enactment of the Affordable Care Act is expected to increase the utilization of these services. A systematic review to evaluate the role of APPs in cancer screening and prevention examined 15 studies published from 1990–2011 (7). When evaluating breast cancer screening practices, studies reviewed showed that 69–91% of patients who saw APRNs received mammograms and that APRNs make mammogram recommendations similarly as physicians. An intervention study compared screening offered and conducted by an APRN during a routine clinic visit to a standard chart reminder system. This showed significantly higher increase in the annual rate of Pap smears and mammograms in the intervention group who received screening during their routine visit, compared to the increase in the annual rate of these screening activities through a chart reminder system (7,17). This supports the thoughtful and systematic use of APP resources in intervention programs that can help improve outcomes. Furthermore, APPs are also valuable resources in interdisciplinary practices for cancer prevention counseling. The systematic review showed that smoking cessation recommendations are provided routinely by both physicians and physician extenders; however, of the nine studies pertaining to tobacco cessation, three showed that patients are more likely to receive recommendations for smoking cessation during visits with APPs than during visits without them (7). With the demands and time constraints on physicians, it is essential to optimize APP utilization to improve screening and prevention programs.
In settings such as MD Anderson Cancer Center, APPs manage APP-staffed screening and prevention outpatient clinics. While physician collaboration and oversight is in place at these practices, APPs optimize their practice scope by providing services that include routine surveillance, screening services and procedures, review of diagnostic studies, education regarding screening practices. In some high-risk patient populations, APPs engage in discussion of chemoprevention options, including providing patients with risk profiles to better equip them to make well-informed decisions about preventative care. The benefits of APP utilization in this setting include improved access to evidence based care as well as cost-effective care. Understanding the scope of practice for APPs and allowing them to make the most of their education, training and skills is essential to optimizing the collaboration of health care givers within the interdisciplinary team.
Treatment and disease management settings
While APPs are of significant value to screening and prevention programs, their skills are most frequently utilized in the active treatment and management of cancer. APPs practice in the inpatient setting, outpatient clinics, and in the operating room. They practice in different clinical specialties within the surgical oncology, medical oncology, and radiation oncology disciplines alongside oncology physicians and other interdisciplinary experts. APPs are involved in reviewing referrals and directing patients to the appropriate clinics for their initial evaluation and diagnostic procedures. They collaborate with physicians to determine treatment decisions, oversee the coordination of care, conduct follow-up visits, and provide symptom management. In carrying out these functions, they are engaged as clinicians, educators, and patient advocates. They also collaborate during treatment and disease management by facilitating clinical trials and other research-related efforts. The 2011 ASCO Study of Collaborative Practice Arrangements noted that patients were satisfied when their care was provided by APPs, and that there was a reported increase in productivity in practices that utilized APPs, and that physicians and APPs are highly satisfied with collaborative practices (3).
In the outpatient setting, APPs facilitate expeditious access for new patients who need evaluation for a newly diagnosed cancer or for a possible cancer diagnosis. There are APPs who work closely with the referral centers in large cancer centers to review cases with referring physicians and direct the patient to the appropriate medical or surgical clinics. APPs sometimes coordinate care with the referring physicians and the patients even before the patient’s first visit. In surgical practices where surgeons have high-volume operative obligations precluding them from being able to conduct clinic consultations daily, their APP partners are available to evaluate patients and arrange appropriate diagnostic and staging tests that can expedite care. The surgeon and the interdisciplinary team can then evaluate and plan treatment with diagnostic information already available following a pre-consultation visit with the APP. In similar cases when surgeons are attending to operative cases, pre-operative and post-operative evaluations can be managed by the APPs. In the peri-operative setting, APPs provide surgical first-assist services by participating in operations ranging from relatively minor skin cancer excisions to major, multi-surgical service resections. In other medical specialties, APPs run fast-track clinics for patients who require lab monitoring and symptom management while on cancer treatment. In addition to managing APP-staffed clinics, they also see new and complex follow-up patients in collaboration with physicians. While APPs have the autonomy to carry out many services and collaborate with other health care providers to manage oncology patients in U.S., the plan for cancer resection, systemic cancer treatment, and radiation treatment requires the final authorization of the physicians whose active involvement and oversight is also required while the plan is implemented.
APPs dedicated to the inpatient setting provide the stability and expertise on the hospital units as they manage clinical concerns, patient education and counseling needs, and overall coordination of care. Many members of the interdisciplinary team including physicians often have outpatient clinic responsibilities or in the case of surgeons, operating room responsibilities so having inpatient APPs present on the hospital units provide the necessary first line presence in managing and coordinating the complicated care for hospitalized cancer patients. A recent retrospective study examined 95 patients with acute myelogenous leukemia (AML) admitted for re-induction chemotherapy from 2008–2012 into either a PA service or a resident service, both of which were overseen and supervised by faculty attending physicians (8). Forty-seven patients were admitted to the resident service while 48 were admitted to the PA service and results revealed equivalent mortality but with a statistically significant difference (P=0.03) in the shorter length of stay for the PA service (mean of 30.9 days) compared to the resident service (mean 36.8 days). The number of consults and the 14-day readmission rate also revealed a statistically significant difference in favor of the PA service (P=0.03). The 14-day readmission rate was 10.6% for the resident service while it was aero for the PA service. The mean number of consults also showed a statistically significant difference (P=0.03) and indicated a 2.11 consults (range, 0–5 consults) for the resident service and 1.47 (range, 0–4) for the PA service. Along with mortality, the ICU transfers did not reveal a significant difference between the two groups of caregivers working with faculty attending physicians (8). In services where physicians and medical trainees have obligations in different areas of the hospitals and clinics, there is support for advantages to having inpatient APPs focused on managing the hospitalized patients. More studies are needed to bear out these findings and examine other advantages of APP services in the acute inpatient management of different cancer patient populations.
The APPs’ work from admission to discharge including post-discharge coordination with the patient’s outpatient care givers is helpful with reducing readmissions, discharge delays, post-discharge clinic drop-in visits, and decreasing complication rates. At MD Anderson Cancer Center, inpatient APPs have also worked with physicians to develop and implement enhanced recovery programs and tele-medicine post-operative programs in an effort to improve surgical outcomes.
Survivorship care
With an increasing number of cancer survivors in the United States as well as a decrease in physicians entering the field of oncology, APPs have been identified as members of the healthcare team that can help balance the oncology supply and demand (McCabe & Pickard, 2012). APPs are trained such that they are well-equipped to provide the comprehensive care proposed for cancer survivors, including ongoing age-specific cancer screening, general wellness, disease prevention, counseling, and management of cancer therapy sequelae. Because of developments in early detection and advances in treatment, the number of cancer survivors in the United States approaches 12 million with an estimated 7.2% of the general population aged 18 or older reporting a personal history of cancer (9). Additionally, many APPs manage APP-staffed clinics in the outpatient setting, which provide surveillance for recurrence, new cancer screening, identification and management of late effects of cancer treatment, and as previously discussed, health prevention measures.
The improvement in cancer therapies and the resulting reduction in mortality rates point to longer time periods that patients will live through the different phases of the disease; thus, contributing to an increased demand for symptom management and survivorship care (9). As such, APPs will be called upon to help reduce the gap in care, and to ensure that effective and efficient survivorship programs are in place to provide optimal patient management.
Palliative care
Services that comprise palliative care include team-based care planning, pain and symptom management, communication with patients and families, ensuring continuity of care across range of clinical settings, attention of spiritual comfort and psychosocial support, bereavement support, and hospice care (Fox, 2014). APPs are not only well-positioned to provide these services but can also benefit the patient and the interdisciplinary team by leading special intervention programs that improve overall care and specific outcomes. A prospective randomized study examined the value of palliative interventions from an advanced registered nurse practitioner compared to standard care for patients with metastatic cancer (18). The investigators found that interventions from advanced practice nurse practitioners that included explanation of hospice benefits and discussion regarding advanced directives early in the course of treatment for metastatic disease lead to measurable, statistically significant improvements in the patients’ reported emotional and mental quality of life (18). APPs can be utilized to lead intervention programs that provide added benefits to alleviate the distress of patients and families receiving end-of-life care.
Summary
The training and education of APPs afford them the special skill set to benefit patients and provide an essential resource to alleviating the burden associated with the projected shortage of oncology clinicians. APPs and physicians in collaborative oncology practices both report high satisfaction with the collaboration, and patients report that they are aware when being treated by an APP and indicate that they are very satisfied with the care they receive in these collaborative oncology practices (3). APPs can enhance the care oncology patients receive through interventions that improve the effective utilization of prevention and screening services as well as promoting high-quality care delivery and outcomes. Looking ahead to the future, APPs can continue their clinical contributions and education efforts to help prepare trainees for oncology care. Additionally, APPs can also enhance their research efforts and look into investigating innovative ways to improve care delivery and the quality of life for patients throughout the cancer illness experience. Information gleaned from these investigations can provide the foundation for advances in interdisciplinary cancer care and research.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Smith BD, Smith GL, Hurria A, et al. Future of cancer incidence in the United States: burdens upon an aging, changing nation. J Clin Oncol 2009;27:2758-65. [Crossref] [PubMed]
- Erikson C, Salsberg E, Forte G, et al. Future supply and demand for oncologists: challenges to assuring access to oncology services. J Oncol Pract 2007;3:79-86. [Crossref] [PubMed]
- Towle EL, Barr TR, Hanley A, et al. Results of the ASCO Study of Collaborative Practice Arrangements. J Oncol Pract 2011;7:278-82. [Crossref] [PubMed]
- American Association of Nurse Practitioners [Internet]. Austin: American Association of Nurse Practitioners: NP Fact Sheet; 2015. [date unknown] Available online: http://www.asco.org/sites/default/files/oncology_workforce_report_final.pdf
- National Commision on Certification of Physician Assistants [Internet]. Duluth: National Commision on Certification of Physician Assistants: 2015 Statistical of Certified Physician Assistants; 2016. Available online: https://www.nccpa.net/Uploads/docs/2015StatisticalProfileofCertifiedPhysicianAssistants.pdf
- Ross AC, Polansky MN, Parker PA, et al. Understanding the role of physician assistants in oncology. J Oncol Pract 2010;6:26-30. [Crossref] [PubMed]
- Smith AA, Kepka D, Yabroff KR. Advanced practice registered nurses, physician assistants and cancer prevention and screening: a systematic review. BMC Health Serv Res 2014;14:68. [Crossref] [PubMed]
- Glotzbecker BE, Yolin-Raley DS, DeAngelo DJ, et al. Impact of physician assistants on the outcomes of patients with acute myelogenous leukemia receiving chemotherapy in an academic medical center. J Oncol Pract 2013;9:e228-33. [Crossref] [PubMed]
- McCabe MS, Pickard TA. Planning for the future: the role of nurse practitioners and physician assistants in survivorship care. Am Soc Clin Oncol Educ Book 2012.e56-61. [PubMed]
- Fox K. The role of the acute care nurse practitioner in the implementation of the commission on cancer's standards on palliative care. Clin J Oncol Nurs 2014;18 Suppl:39-44. [Crossref] [PubMed]
- American Association of Nurse Practitioners [Internet]. Austin: American Association of Nurse Practitioners: State Practice Environment; 2016. [date unknown] Available online: https://www.aanp.org/legislation-regulation/state-legislation/state-practice-environment
- American Academy of Physician Assistants [Internet]. Alexandria: American Academy of Physician Assistants What is a PA?; 2016 [date unknown]. Available online: https://www.aapa.org/what-is-a-pa/?utm_source=aapa.org&utm_medium=blue_buttons&utm_content=what&utm_campaign=homepage
- American Association of Nurse Practitioners [Internet]. Austin: American Association of Nurse Practitioner: Nurse Practitioner Curriculum; 2013. [date unknown] Available online: https://www.aanp.org/images/documents/publications/curriculum.pdf
- Hass V. Physician assistants and nurse practitioners are not interchangeable. JAAPA 2016;29:9-12. [Crossref] [PubMed]
- American Association of Nurse Practitioners [Internet]. Austin: American Association of Nurse Practitioners: What’s an NP?: 2016. [date unknown] Available online: https://www.aanp.org/all-about-nps/what-is-an-np
- The National Organization of Nurse Practitioner Faculties. [Internet]. Washington DC: The National Organization of Nurse Practitioner Faculties: Nurse Practitioner Core Competencies Content; 2014. [date unknown] Available online: http://c.ymcdn.com/sites/nonpf.site-ym.com/resource/resmgr/Competencies/NPCoreCompsContentFinalNov20.pdf
- Mandelblatt J, Traxler M, Lakin P, et al. A nurse practitioner intervention to increase breast and cervical cancer screening for poor, elderly black women. The Harlem Study Team. J Gen Intern Med 1993;8:173-8. [Crossref] [PubMed]
- Dyar S, Lesperance M, Shannon R, et al. A nurse practitioner directed intervention improves the quality of life of patients with metastatic cancer: results of a randomized pilot study. J Palliat Med 2012;15:890-5. [Crossref] [PubMed]


