
Palliative interventions for patients with advanced gastric cancer: a systematic review
Highlight box
Key findings
• Patients with AGC undergo a variety of interventions aimed at palliating the symptoms associated with their diagnosis and improving their QoL.
• Few studies identified by this systematic review measured QoL as a primary outcome, and no studies were qualitative in nature.
What is known and what is new?
• AGC is associated with significant morbidity and mortality and is commonly accompanied by a variety of distressing symptoms.
• Many of the distressing symptoms associated with AGC can be palliated using a variety of multidisciplinary approaches.
What is the implication, and what should change now?
• More work is required to better characterize the patient experience of living with gastric cancer.
• Patient reported outcome measures should be captured in all ongoing and future studies of AGC patients undergoing palliative interventions including palliative surgery.
Introduction
Background and rationale
Gastric cancer is the fifth most common cancer and the third leading cause of cancer-related death worldwide (1,2). In Western countries, the majority of patients with gastric cancer are diagnosed with advanced disease at the time of initial presentation (1,3). Advanced gastric cancer (AGC) is defined as T1b to T4 disease, invading the submucosa, muscularis propria, subserosa, perforating serosa, or invading adjacent structures, without distant metastasis (4). For the purposes of this review, AGC includes unresectable locally advanced, locally recurrent, and metastatic disease. AGC has a poor prognosis overall and is associated with significant morbidity and mortality (5). Patients with AGC may suffer from a variety of distressing symptoms, which typically occur late in disease progression. The most common symptoms include nausea, vomiting, anorexia, weight loss, dyspepsia, abdominal pain, and bleeding (3,5,6).
According to the World Health Organization (WHO), palliative care is “an approach that improves the quality of life of patients and their families facing the problems associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual” (7). The treatment of AGC should be influenced by palliative care principles, which aim to relieve symptoms, improve quality of life (QoL), and aid patients with informed decision-making and advanced care planning (5). Treatment is multimodal and should include an interprofessional team, comprised of surgical, medical, and radiation oncologists, gastroenterologists, palliative care specialists, nurses, and allied care providers (8). Throughout this review, we will refer to interventions as ‘palliative interventions’ including surgery, endoscopy, chemotherapy, radiation therapy, systemic therapy, and supportive care interventions, if they are delivered with the goal of addressing the physical, psychosocial, and spiritual needs of the patient. It should be noted that the decision to pursue a palliative intervention is made by the patient in conjunction with the interprofessional care team, based on a multitude of factors, including the extent of disease, the symptom burden, and importantly, the patient’s goals of care.
Despite palliative care being a relatively well-defined field of study, palliative interventions in gastric cancer are not well characterized and there is significant heterogeneity in the literature defining palliative interventions (6). Previous work has highlighted the need to focus on outcome measures relevant to symptom management and QoL (6). Despite this, most of the research on AGC remains survival-oriented with a focus on outcomes related to survival benefit with a disregard of the patient experience. It is therefore important that health care providers and researchers share common priorities in order to provide individualized and comprehensive care plans for patients with AGC. We present the following article in accordance with the PRISMA reporting checklist (available at https://cco.amegroups.com/article/view/10.21037/cco-22-102/rc).
Objectives
The primary objective of this systematic review was to explore the published literature on palliative interventions for AGC. The secondary objective was to characterize updates in the literature on palliative interventions, specifically focused on the management of common symptoms, QoL, and the psychosocial and spiritual needs of patients with AGC.
Methods
Eligibility criteria
We included English language studies published between January 1, 2010 and August 18, 2022, that investigated palliative interventions for AGC. Palliative interventions were defined as surgery, endoscopy, chemotherapy, radiation therapy, targeted therapy, and supportive care interventions, delivered with the goal of addressing the physical, psychosocial, and spiritual needs of the patient. AGC was defined as T1b to T4 disease, including unresectable locally advanced, locally recurrent, and metastatic cancer.
Inclusion and exclusion criteria
We included primary literature in the form of clinical trials, cohort studies, case-control studies, and case series. We excluded studies according to the following exclusion criteria: (I) unpublished research (i.e., conference abstracts only), (II) secondary literature (i.e., review articles), (III) studies not focused on patients with AGC, (IV) studies with outcome measures that were not associated with the relief of symptoms or improvement in QoL, (V) case reports and/or studies with less than ten patients, (VI) studies on mixed cancer types, with either less than 50% gastric cancer patients or an undefined patient population. Studies with less than 10 patients and those with <50% of cases with AGC were excluded as we felt that the findings from such studies would not be generalizable. A summary of the search strategy is outlined in Table 1.
Table 1
| Items | Specification |
|---|---|
| Date of search | August 19, 2022 |
| Databases and other sources searched | PubMed, EMBASE, Cochrane Library, manual search |
| Search terms used | Mesh terms: Stomach neoplasms, palliative care, hospice and palliative care nursing, hospice care, terminal care, advanced care planning, palliative medicine |
| Free text search terms: Gastric, stomach, cancer, neoplasm, adenocarcinoma, carcinoma, tumor, tumour, malign*, palliat*, hospice, advanced care, end of life, terminal, advanced medical plan, advanced health care plan, hyperthermic intraperitoneal chemotherapy*, HIPEC, endoscopic intervention, endoscopic treatment, endoscopy intervention*, endoscopy treatment | |
| Timeframe | January 1, 2010–August 18, 2022 |
| Inclusion and exclusion criteria | Inclusion criteria |
| English language studies published between January 1, 2010, and August 18, 2022 | |
| Studies that investigated palliative interventions for AGC | |
| Primary literature, in the form of clinical trials, cohort studies, case-control studies, and case series studies | |
| Exclusion criteria | |
| Unpublished research | |
| Secondary literature | |
| Studies with the wrong patient population | |
| Studies with the wrong outcome measure | |
| Case reports with less than ten patients | |
| Studies on mixed cancer types, with either less than 50% gastric cancer patients or an undefined population | |
| Selection process | Two reviewers (KK and OM) independently screened all titles and abstracts. Conflicts were discussed by the two reviewers until agreement was achieved. Two reviewers (KK and OM) conducted full-text review |
AGC, advanced gastric cancer.
Information source, selection process, and search strategy
An informationist from Welch Medical Library at Johns Hopkins University developed and conducted the literature searches with team input. We searched PubMed, Embase, and Cochrane Library to identify studies published within our timeframe of interest. We developed our search strategies using a combination of controlled vocabulary and keywords to define the concepts of gastric cancer and palliative care interventions. References from included studies and review articles were hand-searched to identify any additional relevant studies for analysis. The PubMed search is outlined in Table S1.
Data collection process
Search results from each database were imported into Covidence systematic review software (9) to remove duplicate records and facilitate screening. Two reviewers (KK and OM) independently screened all titles and abstracts. Conflicts were discussed by the two reviewers until agreement was achieved. Two reviewers (KK and OM) conducted the full-text review and independently extracted and verified data points to be included in the manuscript.
Data items and synthesis method
We identified and abstracted the following data points from all included studies: number of participants, study design, and treatment modality (Table 2). Based on the data abstraction, we created a concept map, generated the included tables, and synthesized the conclusions from the selected articles. Meta-analysis was not performed given the heterogeneity of the included interventions.
Table 2
| Data items | Outcome parameters |
|---|---|
| Number of participants | Integers greater than 10 (i.e., denoting at least ten participants or more) |
| Study design | Clinical trials, cohort studies, case-control studies, and case series |
| Treatment modality | Surgery, endoscopic intervention, radiation, chemotherapy, arterial embolization, medication, supplemental nutrition, ablation, rotary magnetic fields, specialty palliative care consultation, advanced care planning, hospice services |
Quality assessment
As recommended by Ma et al. (10) we included various validated quality assessment tools for our quality assessment, including the NIH Quality Assessment Tool for Case Series Studies to assess case series studies (11), the Critical Appraisal Skills Programme worksheets to assess cohort and case control studies (12), the ROBINS-I tool to assess non-randomized clinical trials (13), and the Cochrane Risk of Bias Tool for Randomized Controlled Trials (14) to assess randomized controlled trials. Using the assessment tools outlined above, we assigned overall quality ratings of high, moderate, low, or very low based on the study design and risk for bias.
Results
Our search results are reported in accordance with the PRISMA 2020 statement (15) (Figure 1). We identified 10,361 studies from our systematic database search, including 3,631 PubMed, 6,209 EMBASE, and 521 Cochrane Library records, in addition to 3 studies identified through manual review. We identified 2,918 duplicates, which were removed before screening. We screened a total of 7,446 studies by title and abstract review, of which 7,292 studies were excluded. We sought retrieval of 154 studies. Fifteen studies were not able to be retrieved in full text and were therefore excluded; no attempt was made to contact authors directly. We assessed 139 studies for eligibility through full-text review, of which 73 were studies excluded. We included 66 studies in our review.
In total, 66 full-text publications met our inclusion criteria and were included for final review. Twenty-three studies addressed the palliative management of bleeding in AGC, with radiation therapy being the most studied modality for bleeding control. Twenty-two studies addressed the management of obstructive symptoms in AGC including nausea, vomiting, anorexia, and dyspepsia, secondary to obstruction. Interventions aimed to ameliorate both proximal [gastroesophageal junction (GEJ)] and distal (gastric outlet) obstruction were included. Five publications assessed modalities to reduce the burden of symptomatic intraabdominal ascites, including hyperthermic intraperitoneal chemotherapy (HIPEC) and systemic chemotherapeutics. A total of 15 studies assessed QoL in a spectrum of patient populations, including those receiving chemotherapy, radiotherapy, supplemental nutrition, and procedural interventions, including surgery. Only five of these studies used QoL as a primary outcome, while ten studies reported QoL as a secondary outcome. Only one study evaluated specialty palliative care consultation for patients with AGC, and no studies outlined the prevalence or practices of advanced care planning for this patient population.
Bleeding
Symptom description
Bleeding caused by AGC occurs due to uncontrolled tumor growth, which can result in anemia and numerous related symptoms. Patients may experience hematemesis or have melanotic stools. Bleeding and anemia contribute to the related symptoms of fatigue, weakness, and shortness of breath. Uncontrolled bleeding can cause severe symptoms, including dizziness, light-headedness, and syncope, secondary to hypotension. Without hemostasis, uncontrolled bleeding can be life-threatening.
Treatment modalities
Described treatment modalities for bleeding in AGC include radiation, surgical or endoscopic interventions including the application of topical hemostatic agents, transcatheter arterial embolization (TAE), and chemotherapy (see Table 3 and Figure 2).
Table 3
| Modality | Year | Title | Study design | N | Intervention | Conclusion | Overall quality rating |
|---|---|---|---|---|---|---|---|
| Radiation | 2012 | Palliative haemostatic radiotherapy for advanced cancer of the stomach (16) | Retrospective case series, single institution | 28 | External beam radiotherapy, with ranges of 22.5 Gy over 5 fractions to 40 Gy over 20 fractions; BED of 32.6–48 Gy | Rate of bleeding control was 65.2% with median duration of response of 60 days (range, 11 to 479 days) | Moderate |
| Radiation | 2011 | Palliative radiotherapy for bleeding from advanced gastric cancer: is a schedule of 30 Gy in 10 fractions adequate? (17) | Retrospective case series, single institution | 30 | Short-course radiotherapy with 30 Gy in 10 fractions | Rate of bleeding control was 50% of patients treated with this regimen | Moderate |
| Radiation | 2018 | Efficacy of palliative radiotherapy and chemo-radiotherapy for unresectable gastric cancer demonstrating bleeding and obstruction (18) | Retrospective case series, single institution | 23 | Median total dose and fraction in this patient population was 42 Gy over 20 fractions | Response rate to resolution of bleeding was 88.8% | Low |
| Radiation | 2022 | Palliative radiotherapy for bleeding from unresectable gastric cancer using three-dimensional conformal technique (19) | Retrospective case series, single institution | 20 | Median first radiation dose was a BED of 39.9 Gy | Treatment success rate was 95% and the re-bleeding rate was 10.5%; two patients were re-irradiated for hemostasis and gastrointestinal perforation occurred in both patients | Moderate |
| Radiation | 2014 | The role of palliative radiotherapy for haemostasis in unresectable gastric cancer: a single-institution experience (20) | Retrospective case series, single institution | 52 | 75% of patients received a single 8 Gy fraction, and 25% of patients received 20 Gy in 5 fractions | 50% of patients required fewer blood transfusions within 4 weeks of radiotherapy | High |
| Radiation | 2021 | Efficacy of radiotherapy for gastric bleeding associated with advanced gastric cancer (21) | Retrospective case series, single institution | 57 | The median BED was 37.5 Gy; the most common regimen was 25 Gy in 5 fractions | Mean hemoglobin was significantly higher after radiation therapy | Moderate |
| Radiation | 2021 | Hemostatic effect of palliative radiation therapy in preventing blood transfusions from bleeding occurring within advanced gastric cancer (22) | Retrospective case series, single institution | 28 | Patients were treated with 30 Gy in 10 fractions or 40 Gy in 20 fractions | No statistically significant decrease in hemoglobin level was observed 4 weeks after radiotherapy; 1-year blood-transfusion free survival was significantly higher in patients treated with 30 Gy in 10 fractions compared with patients treated with 40 Gy in 20 fractions | Moderate |
| Radiation | 2017 | Palliative external beam radiotherapy for the treatment of tumor bleeding in inoperable advanced gastric cancer (23) | Retrospective case series, single institution | 42 | Radiotherapy was delivered with a median total dose of 39.6 Gy in a median number of 20 fractions | The palliation of gastric tumor bleeding was achieved in 69% of patients; the BED for responders was significantly higher than the BED for non-responders (48 vs. 26.4 Gy) with a calculated optimal cut off value of 36 Gy | Moderate |
| Radiation | 2022 | Verification of the utility of palliative radiotherapy for hemostasis of gastric cancer bleeding: a case control study (24) | Retrospective case series, single institution | 33 | 76% of patients received a BED of 39 and 24% of patients received a BID of <39 | Hemostasis was achieved in 73% of patients | Moderate |
| Radiation | 2022 | Palliative radiotherapy for gastric cancer bleeding: a multi-institutional retrospective study (25) | Retrospective case series, multi-institutional | 117 | 30 Gy in 10 fractions delivered over a period of 2 weeks was considered as standard treatment, but physicians decided the treatment dose for each patient with consideration of the patients’ condition, tumor pathology, and treatment history | Overall rate of achievement of hemostasis was 59.6% | Moderate |
| Radiation | 2014 | Clinical outcome of palliative radiotherapy for locally advanced symptomatic gastric cancer in the modern era (26) | Retrospective case series, single institution | 115 | 60% of patients received a BED less than 39; 40% of patients received a BED greater than 39 | Response rate for bleeding was 80.6% | Moderate |
| Radiation | 2019 | Palliative radiotherapy in symptomatic locally advanced gastric cancer: a phase II trial (27) | Non-randomized clinical trial | 50 | 36 Gy in 12 daily fractions, 5 days a week equating to a BED of 48.6 Gy | 80% of patients responded to radiotherapy | High |
| Radiation | 2021 | Role of palliative radiotherapy in bleeding control in patients with unresectable advanced gastric cancer (28) | Retrospective case series, single institution | 61 | Median dose was 30 Gy, with a daily dose ranging from 1.8 to 3 Gy | 88% of patients achieved bleeding control after radiotherapy | Moderate |
| Radiation | 2015 | Efficacy of palliative radiotherapy for gastric bleeding in patients with unresectable advanced gastric cancer: a retrospective cohort study (29) | Retrospective case series, single institution | 17 | The median total planned radiation dose was 30 Gy in 10 fractions | The median hemoglobin level before radiotherapy significantly increased from 6.0 to 9.0 g/dL; the median volume of red blood cell transfusion significantly decreased from 1,120 to 280 mL and the median re-bleeding-free survival interval was 27 days | Moderate |
| Radiation | 2022 | Temporal profiles of symptom scores after palliative radiotherapy for bleeding gastric cancer with adjustment for the palliative prognostic index: an exploratory analysis of a multicentre prospective observational study (JROSG 17-3) (30) | Prospective cohort study, single institution | 55 | The median 20 Gy total radiation dose was delivered in a median of 5 fractions; most patients received either 8 Gy in one fraction (21%), 20 Gy in 5 fractions (32%) or 30 Gy in 10 fractions (38%) | Shortness of breath, pain and distress significantly improved; an improvement in fatigue and distress was observed only in patients treated with a BED | Moderate |
| Radiation | 2017 | Experience of low-dose, short-course palliative radiotherapy for bleeding from unresectable gastric cancer (31) | Retrospective case series, single institution | 18 | 6 Gy in 3 fractions | The treatment success rate at 2 weeks after radiation was 55%; there was a statistically significant increase in the mean hemoglobin level and a significant decrease in the mean number of transfused red blood cell units at 1 month | Moderate |
| TAE | 2017 | Transcatheter arterial embolization for gastrointestinal bleeding associated with gastric carcinoma: prognostic factors predicting successful hemostasis and survival (32) | Retrospective case series, single institution | 43 | TAE; for patients with positive angiographic findings, selective embolization was performed with n-butyl cyanoacrylate or micro-coils. When angiography showed no abnormal findings, empirical embolization was performed | Technical and clinical success rates of TAE were 85.0% and 65.0% | Moderate |
| TAE | 2020 | Transcatheter arterial embolization for advanced gastric cancer bleeding: a single-center experience with 58 patients (33) | Retrospective case series, single institution | 58 | TAE; all patients with positive angiograms underwent selective embolization treatment. Those with negative angiography findings underwent empirical embolization | Technical success was achieved in 100% of the procedures, while the overall clinical success rate was 72.4%; the success rate for patients with positive angiography was 53.8% | Moderate |
| Endoscopy | 2013 | Outcome of endoscopic therapy for cancer bleeding in patients with unresectable gastric cancer (34) | Retrospective case series, single institution | 113 | Endoscopic therapy for upper gastrointestinal bleeding secondary to unresectable AGC; electrocoagulation was the most common method used (92.0%) | The initial hemostasis rate was 92.9% and electrocoagulation was the most common method used. The initial hemostasis rate of clipping was 70% and patients with active spurting had the lowest rate of initial hemostasis (82.4%). Re-bleeding occurred in 41.0% of all patients; 3- and 30-day re-bleeding rates were 18.1% and 29.5%, respectively | Moderate |
| Endoscopy | 2013 | The successful endoscopic hemostasis factors in bleeding from advanced gastric cancer (35) | Retrospective cohort study, single institution | 45 | Endoscopists chose the hemostatic method most appropriate to the clinical situation, including epinephrine injection, epinephrine spray, hemoclipping, or argon plasma coagulation based on the patient’s hemorrhagic site and clinical conditions | 86.7% of patients had lesions larger than 2 cm. Lesion size and bleeding condition were statistically significant predictive factors for endoscopic hemostatic failure; lesion size >2 cm was a significant predictive factor for endoscopic hemostatic failure | Low |
| Chemotherapy | 2020 | Efficacy of chronomodulated chemotherapy for palliation of hematemesis in inoperable gastric cancer: a single-institutional retrospective study (36) | Retrospective case series, single institution | 70 | Every 3-week chronomodulated treatments of epirubicin and oxaliplatin for a total of six cycles | At 12-week follow-up, there was a significant decrease in mean average episodes of emesis per week as compared to baseline, from an average of 2.7 episodes of hematemesis per week to 1.5 for the entire cohort | Moderate |
| Medication | 2017 | Effect of a proton pump inhibitor on tumor bleeding prevention in unresectable gastric cancer patients: a double-blind, randomized, placebo-controlled trial (37) | Randomized-controlled trial | 127 | Patients with inoperable gastric cancer were randomly assigned to receive oral lansoprazole (30 mg) or placebo daily | During the median follow-up of 6.4 months, tumor bleeding rates were 7.8% and 9.5%, in the lansoprazole and placebo groups, respectively, (not statistically different). However, during the initial 4 months, 4 placebo-treated patients developed tumor bleeding, whereas there were no bleeding events in the lansoprazole-treated patients | High |
| Surgery versus radiation | 2022 | Clinical outcomes of palliative treatment for gastric bleeding from incurable gastric cancer (38) | Retrospective cohort study, single institution | 48 | 23 patients underwent palliative surgery and 25 patients underwent palliative radiotherapy | 88% of patients achieved hemostasis, but re-bleeding was noted in 40%; severe complications were observed in 8.6% of patients after palliative surgical intervention | Moderate |
AGC, advanced gastric cancer; BED, biologically effective dose; BID, twice daily; TAE, transcatheter arterial embolization.
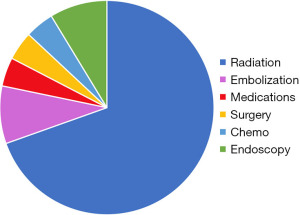
Radiation
All but one of the published studies regarding the use of radiation therapy for the management of bleeding secondary to AGC was a retrospective case series or case-control study, with only one non-randomized clinical trial intervention studied (16-22,24-26,28-31,39). The most common treatment regimen was 30 Gy in 10 fractions ranging from a single 8 Gy fraction dose to 42 Gy over 20 fractions. Some studies, but not all, reported biologically equivalent doses (BEDs). Most studies assessed post-intervention success by the absence of re-bleeding within a defined time period, though some authors reported the need for post-procedural transfusion or changes in the post-procedural hemoglobin levels as a surrogate for reduction in tumor bleeding. The range of response rates to the varying doses of radiation was 50–89.5%. In contrast, Kawamoto et al. focused solely on symptoms as a primary outcome and demonstrated that shortness of breath, pain, and distress improved after radiotherapy (30). At least two studies reported on the use of repeat radiotherapy doses in an attempt to control re-bleeding (19,31). In one of these studies (31), two patients were re-irradiated for hemostasis, and, unfortunately, gastrointestinal perforation occurred in both patients.
TAE
Two studies retrospectively analyzed the use of TAE for bleeding secondary to AGC (32,33). In both studies, all patients with positive angiograms underwent selective embolization, and those with negative angiography underwent empirical embolization. Both studies report technical and clinical success rates. Park et al. noted a clinical success rate of 65%, and found that the median interval between TAE and re-bleeding was 16 days (32). Cho et al. had a higher clinical success rate of 72.4%, though the primary endpoint was measured 14 days after embolization (33).
Endoscopy
Two studies reported on endoscopic interventions for patients with AGC (34,40). Kim et al. focused on assessing success rates for each intervention type, which included electrocoagulation and clipping, or combination therapy, where more than one technique was required to achieve hemostasis (34). Contrarily, Koh et al. (35) characterized the differences in the gastric lesions themselves as predictive factors for the success of hemostatic therapeutic interventions. Both studies reported the Forrest Classification to describe the stigmata of recent hemorrhage (40).
Chemotherapy
A single study by Biswas et al. reported the efficacy of chronomodulated treatments of epirubicin and oxaliplatin every 3-week, for a total of six cycles (36). Chronomodulation refers to the practice of administering anticancer drugs at specific times of the day to exploit the circadian variation in drug response. To assess response to treatment, the team formulated a scoring system to quantify upper gastrointestinal bleeding, termed the “average episodes per-week” score, or AEP score, which was defined as the total number hematemesis episodes experienced in the last 6 weeks divided by six. Hemoglobin levels and the number of required transfusions over the treatment period were used to quantify the severity of the blood loss. At 12-week follow-up, the authors identified a significant decrease in average episodes of hematemesis per week, from 2.7 episodes of hematemesis per week to 1.5 for the entire cohort.
Medication
The only study that assessed the use of medication in the management of bleeding secondary to inoperable gastric cancer was a prospective double-blind, randomized, placebo-controlled trial, which studied the effects of proton pump inhibitor (PPI) treatment on the prevention of tumor bleeding (37). For this study, 127 patients with inoperable gastric cancer were randomly assigned to receive oral Lansoprazole (30 mg) or placebo daily. The authors found that during the median follow-up of 6.4 months, tumor bleeding rates were 7.8% in the Lansoprazole group compared to 9.5% in the placebo group however this difference was not statistically significant. The authors concluded that Lansoprazole did not significantly reduce the incidence of tumor bleeding, and recommended that future studies focus on the effects of PPI therapy on tumor bleeding during the earlier phases of chemotherapy.
Comparative outcomes
One retrospective analysis assessed the treatment outcomes of patients with AGC who underwent palliative surgery or palliative radiotherapy for bleeding (38) (see Table 2 and Figure 2). Of the 48 patients, 23 underwent palliative surgery (69.6% total gastrectomy, 26.1% distal gastrectomy), and 25 received palliative radiation therapy (median dose of 39 Gy). Post-operative complications (Clavien-Dindo grade II or higher) were reported in 26.1% of patients receiving surgery. For the radiation group, re-bleeding was noted in 40% of patients within 30 days of completing radiotherapy, and no severe adverse events were observed. Chemotherapy was introduced in 91.3% of patients having received palliative surgery, and 68% of patients having received palliative radiation. Overall, the authors recommended consideration of palliative surgery for chemo-naïve patients in good general condition, and radiation therapy for patients in poor general condition or those who have already received chemotherapy.
Obstruction
Symptom description
The symptoms of obstruction secondary to AGC include nausea, vomiting, weight loss, early satiety, dehydration, malnutrition, epigastric pain, and occasionally jaundice or ureteral obstruction. Obstruction can be secondary to obstruction at the GEJ, presenting with symptoms of dysphagia, or gastric outlet obstruction (GOO), leading to nausea and vomiting.
Treatment modalities
Described treatment modalities for the management of obstruction secondary to AGC include endoscopic stenting and surgical interventions, including incomplete or partial tumor resection (R1 or R2), gastrojejunostomy, partial stomach-partitioning gastrojejunostomy, small intestine or colonic bypass, and ileostomy or colostomy creation (Table 4). Of note, studies were identified on the topic of endoscopic ultrasound-guided gastrojejunostomy but were not included as they did not meet our inclusion criteria. No studies described percutaneous endoscopic gastrostomy tube placement in AGC.
Table 4
| Different types of stents |
| Self-expandable metallic stents |
| Custom made and standard sizing |
| Covered, uncovered, and partially covered |
| Different types of surgeries |
| Incomplete or partial tumor resection, R1 or R2 |
| Gastrojejunostomy as a bypass |
| Partial stomach-partitioning gastrojejunostomy |
| Small intestine or colonic bypass |
| Ileostomy or colostomy |
| Laparoscopic versus open |
AGC, advanced gastric cancer.
Stenting
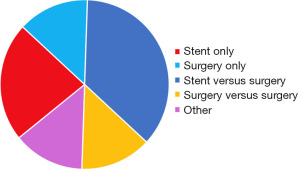
Five studies described palliative endoscopic stenting for patients with AGC, including covered and uncovered endoscopically placed self-expandable metal stents (SEMS) of both custom and standard designs (see Table 5 and Figure 3) (41-45). All studies assessed outcomes after placement of an endoscopic SEMS. Most of the studies assessed stent patency and clinical success using the Gastric Outlet Obstruction Scoring System (GOOSS) (63,64). The GOOSS assigns a scores for no oral intake, liquids only, soft solids, and low-residues or full diet, and currently is the most widely used scoring system to quantify the clinical improvement of patients treated for malignant GOO (64,65). Clinical success was achieved in 82–95% of patients undergoing endoscopic stenting. Kim et al. demonstrated that the technical and clinical success rates of endoscopic stenting were worse for patients with obstruction at the GEJ (technical success rate of 97.6%, clinical success rate of 83.3%), compared to GOO (technical success rate of 98.5%, clinical success rate of 88.8%) (45). Overall, the mean stent patency ranged from 86–158 days (43,45). Endo et al. reported that 72% of patients in their series were able to receive chemotherapeutics after stenting (41).
Table 5
| Category | Year | Title | Study design | N | %* | Intervention | Conclusion | Overall quality rating |
|---|---|---|---|---|---|---|---|---|
| Stent | 2014 | Efficacy of endoscopic gastroduodenal stenting for gastric outlet obstruction due to unresectable advanced gastric cancer: a prospective multicenter study (41) | Non-randomized clinical trial, multi-institutional | 18 | 100% | Placement of an endoscopic self-expandable metallic stent | Stent placement was successfully performed in all patients, with no complications. After stenting, an improvement in the GOOSS score by one or more points was obtained in 94% of patients. Chemotherapy was administered after stenting in 72% patients | Moderate |
| Stent | 2016 | Endoscopic self-expandable metallic stenting for palliation of malignant gastric outlet obstruction in Southeast Asia (42) | Retrospective case series, single institution | 24 | 75% | Placement of an endoscopic self-expandable metallic stent | Technical success rate was 100% with a clinical success rate of 87.5%. All patients resumed oral intake of liquids within the same day of stent placement. There was a significant improvement of GOOSS from 0.6 before stent placement to 2.0 after stent placement | Moderate |
| Stent | 2013 | Self-expandable metallic stent placement in the palliative treatment of malignant obstruction of gastric outlet and duodenum (43) | Retrospective case series, single institution | 30 | 80% | Placement of an endoscopic self-expandable metallic stent | Symptoms improved in 82.7% post-procedure and this was statistically significant. Tumor ingrowth and/or overgrowth were seen in 13.3%, and a second stent was inserted in these patients. The mean stent patency was 100 days | Moderate |
| Stent | 2013 | Individualization of metal stents for management of gastric outlet obstruction caused by distal stomach cancer: a prospective study (44) | Non-randomized clinical trial, multi-institutional | 37 | 100% | Placement of individualized metal stents; cup or funnel shaped with varying lengths | Technical and clinical success was achieved in 97.3% and 94.4% of patients, respectively. There were no procedure-related perforations or deaths | Moderate |
| Stent | 2020 | Self-expandable metal stent of esophagogastric junction versus pyloric area obstruction in advanced gastric cancer patients: retrospective, comparative, single-center study (45) | Retrospective cohort study, single institution | 108 | 100% | Placement of an endoscopic self-expandable metallic stent | This study compared patients with esophagogastric junction or pyloric obstruction. For the EGJ patients, technical success was 97.6% with clinical success rate of 83.3%; for the pyloric obstruction, technical success was 98.5% with a clinical success rate of 88.8%. GOOSS scores were not significantly different between the groups before and after SEMS placement. The average duration stent patient for patients with EGJ obstruction group was 158 days, compared to 86 days for the pyloric obstruction group | Low |
| Surgery | 2017 | Modified Devine exclusion for unresectable distal gastric cancer in symptomatic patients (46) | Retrospective case series, single institution | 10 | 100% | Gastric partitioning with gastrojejunostomy, aka modified Devine exclusion | This procedure was performed for both obstruction and bleeding (60% and 40% of patients respectively. Early oral tolerance and a low rate of blood transfusions were observed postoperatively; there was no postoperative mortality and a very low complication rate without anastomotic leakage. Average hospital stay was 13 days | Very low |
| Surgery | 2021 | QOL assessment after palliative surgery for malignant bowel obstruction caused by peritoneal dissemination of gastric cancer: a prospective multicenter observational study (47) | Prospective case series, multi-institutional | 63 | 100% | Small intestine/colon resection or small intestine/colon bypass or ileostomy/colostomy for bowel obstruction due to peritoneal dissemination of gastric cancer | Symptoms showed statistically significant improvement from baseline; 67% of patients were able to eat solid food 2 weeks after surgery and 57% tolerated oral intake for 3 months | High |
| Surgery | 2011 | Optimal indications of surgical palliation for incurable advanced gastric cancer presenting with malignant gastrointestinal obstruction (48) | Retrospective case series, single institution | 53 | 100% | Non-curative surgical interventions including gastrojejunostomy, bypass, intestinal resection, and ostomy creation | 64% of patients demonstrated a QOL improvement as defined by oral intake improvement, hospital discharge, and implementation of chemotherapy | Moderate |
| Stent after surgery | 2011 | Self-expandable metallic stent placement for malignant obstruction in patients with locally recurrent gastric cancer (49) | Retrospective case series, single institution | 15 | 100% | Placement of an endoscopic self-expandable metallic stent (covered or uncovered) in patients with recurrent gastric cancer after curative-intent subtotal or total gastrectomy | Technical success was achieved in 92% and clinical success occurred in 90%. The GOOSS score at increased at 1 week (from 0.45 to 2.06) and was maintained up to 1 month. Complications occurred in 44% of cases and included 2 perforations, 3 migrations, and 12 re-stenoses. Median stent patency duration was 10.7 weeks | Moderate |
| Stent after surgery | 2014 | Metallic stent placement in patients with recurrent malignant obstruction in the surgically altered stomach (50) | Retrospective cohort, single institution | 196 | 100% | Placement of an endoscopic self-expandable metallic stent (including fully covered stents, a fully polyurethane-covered retrievable stent, polytetrafluoroethylene-covered retrievable stent, and a partially covered dual stent) in patients who had previously undergone surgery for gastric cancer | Technical and clinical success was achieved in 97% and 95.8% of patients respectively. The mean dysphagia score improved from 3.24 to 1.48. The complication rate was 25%. Incidence of stent migration was significantly higher in fully covered stents and in patients who underwent chemotherapy | Moderate |
| Stent versus surgery | 2021 | Palliative surgery or metallic stent positioning for advanced gastric cancer: differences in QOL (51) | Prospective cohort study, single institution | 27 | 100% | Endoscopic placement of SEMS versus open stomach-partitioning gastrojejunostomy | At 1-month, index values showed a statistically significant deterioration of the QoL in patients who underwent surgery when compared to those who underwent SEMS placement. No differences among the groups were recorded at 3-month; at 6-month, the index values showed a statistically significant deterioration of the QoL in patients who underwent SEMS placement | Low |
| Stent vs. surgery | 2012 | Self-expanding metal stents versus antrectomy for the palliative treatment of obstructive adenocarcinoma of the gastric antrum (52) | Retrospective cohort study, single institution | 39 | 100% | Endoscopic placement of SEMS versus antrectomy and Roux-en-Y gastrojejunostomy | There was a statistically significant difference between groups regarding time to oral intake, 1 vs. 4.9 days, for stent placement versus surgery. In-hospital stay was shorter for stent placement as compared to surgery at 1 vs. 7.8 days. Patients undergoing stent placement had a lower rate of post-procedural complications | Low |
| Stent vs. surgery | 2020 | Treatment option of endoscopic stent insertion or gastrojejunostomy for gastric outlet obstruction due to gastric cancer: a propensity score-matched analysis (53) | Retrospective cohort study, multi-institutional | 85 | 100% | Endoscopic placement of SEMS versus gastrojejunostomy | After propensity score matching, the frequency of postoperative complications was significantly less in stent patients 3% compared to gastrojejunostomy patients 21%. A low residue or full diet was achieved by 97% of stent patients and 97% of gastrojejunostomy patients | Moderate |
| Stent vs. surgery | 2013 | Gastric outlet obstruction in gastric cancer: a comparison of three palliative methods (54) | Retrospective cohort study, single institution | 97 | 100% | Endoscopic placement of SEMS, non-curative intent resection, and gastrojejunostomy | Compared to surgery, endoscopic stenting resulted in a faster improvement on oral intake and symptom relief along with a shorter hospitalization. Complication rates, hospital re-admissions, occurrence of biliary obstruction, and the number of patients receiving chemotherapy were similar. The median symptom-free interval was longest in the palliative resection group | High |
| Stent vs. surgery | 2016 | Factors leading to improved results for endoscopic stenting for metastatic antropyloric adenocarcinoma. a comparison with gastrojejunostomy (55) | Prospective cohort study, single institution | 100 | 100% | Endoscopic placement of covered or uncovered metallic stent versus open gastrojejunostomy | Hospital stay and time to resume oral feeding was shorter in patients who had endoscopic stenting versus. Uncovered stents had lower rates of post-operative complications compared to covered stents | Moderate |
| Stent vs. surgery | 2013 | Long-term outcome of palliative therapy for gastric outlet obstruction caused by unresectable gastric cancer in patients with good performance status: endoscopic stenting versus surgery (56) | Retrospective cohort study, single institution | 113 | 100% | Endoscopic placement of SEMS versus gastrojejunostomy | The technical and clinical success rates between the two groups were equivalent as was the incidence of early adverse events. The rate of late adverse events was significantly higher in the stenting group, 44.4%, compared to gastrojejunostomy, 12.2% and the median patency duration was shorter | Low |
| Stent vs. surgery | 2017 | Palliative gastrojejunostomy versus endoscopic stent placement for gastric outlet obstruction in patients with unresectable gastric cancer: a propensity score-matched analysis (57) | Retrospective cohort study, single institution | 144 | 100% | Endoscopic placement of SEMS versus gastrojejunostomy | In a propensity-matched analysis, clinical success rates were comparable between the surgery and stenting groups (95.6 and 96.0%). The stenting group showed significantly shorter hospital stays than the surgery group and the surgery group showed a significantly longer reintervention period. Surgery was identified as an independent protective predictor against reintervention | Moderate |
| Stent vs. surgery | 2016 | Gastroduodenal stent placement versus surgical gastrojejunostomy for the palliation of gastric outlet obstructions in patients with unresectable gastric cancer: a propensity score-matched analysis (58) | Retrospective cohort study, single institution | 224 | 100% | Endoscopic placement of SEMS versus gastrojejunostomy | With the use of propensity-score matching, the dysphagia score was significantly better in the stent group compared to the surgery group at 7 days. Symptom-free duration and hospitalization were significantly longer in the surgery group and the recurrence rate was significantly higher in the stent group | High |
| Surgery vs. surgery | 2017 | Laparoscopic gastrojejunostomy for patients with unresectable gastric cancer with gastric outlet obstruction (59) | Retrospective cohort study, single institution | 53 | 100% | Open versus laparoscopic gastrojejunostomy | Open gastrectomy had a higher rate of postoperative delayed gastric emptying compared to the laparoscopic group (26.1% vs. 0%). The median time to resumption of oral feeding was 4 days after open surgery vs. 2 days after laparoscopic surgery | Moderate |
| Surgery vs. surgery | 2019 | A study of clinical presentation and management of malignant gastric outlet obstruction (Northeast India-based single-centre experience) (60) | Retrospective cohort study, single institution | 107 | 93% | Non-curative intent gastrectomy versus gastrojejunostomy | In both patient populations there was improvement in the GOOSS score in most of the patients after gastrojejunostomy with acceptable patency rates at the end of 90 days | Low |
| Surgery vs. surgery | 2019 | Gastric partitioning for the treatment of malignant gastric outlet obstruction (61) | Retrospective cohort study, single institution | 60 | 100% | Gastric partitioning with gastrojejunostomy or Roux-en-Y versus gastrojejunostomy | The oral acceptance of soft solids and low residue or full diet were achieved by 93.3% of patients who had undergone gastric partitioning patients versus 75.9% of patients who had undergone gastrojejunostomy. There were no differences in postoperative complications and surgical mortality between groups | Low |
| Surgery vs. no surgery | 2014 | Gastrectomy in advanced gastric cancer effectively palliates symptoms and may improve survival in select patients (62) | Retrospective cohort study, single institution | 210 | 100% | Gastrectomy, exploration without resection, and no surgery (n=45) | Symptoms successfully resolved after gastrectomy in 48% with a complication rate of 32% and mortality of 6%. R2 gastrectomy improved abdominal pain in 44% of patients and nausea/vomiting in 40% and this was significantly better than exploration without resection. Postoperative complications were significantly more common following an R2 gastrectomy, resulting in longer total and ICU length of stay. Patients without postoperative complications had an 82.5% higher rate of symptom resolution than patients who developed complications | Low |
*, % denotes the percent of patients with AGC. AGC, advanced gastric cancer; GOOSS, Gastric Outlet Obstruction Scoring System; EGJ, esophagogastric junction; SEMS, self-expandable metal stent; QoL, quality of life; ICU, intensive care unit.
Surgery
Three studies evaluated surgical interventions for patients with AGC (46-48). One study assessed gastric partitioning with gastrojejunostomy in patients presenting with both obstruction and/or bleeding. The authors noted early oral tolerance and an average hospital stay of 13 days (46). In a second study, the target population was comprised of patients with histologically proven gastric adenocarcinoma who presented with bowel obstruction due to peritoneal dissemination. Surgical intervention in this study consisted of a combination of segmental enterectomy, segmental colectomy, ileostomy, and colostomy, depending on the specific clinical scenario (47). In this group of patients, symptoms showed statistically significant improvement from baseline, with 67% of patients able to eat solid food 2 weeks after surgery and 57% of patients able to tolerate oral intake for 3 months. The final study that evaluated surgical interventions for AGC was a retrospective case series study of patients who presented with obstruction caused by primary unresectable or incurable recurrent gastric cancer. The patients in this study underwent either surgical gastrojejunostomy, small bowel or colonic bypass, intestinal resection, or ostomy creation. The authors found that 64% of patients demonstrated a QoL improvement as defined by oral intake improvement, hospital discharge, and ability to start chemotherapy.
Stent after surgery
Two retrospective studies evaluated the efficacy of endoscopic stenting in patients with AGC who had previously undergone curative-intent partial or total gastrectomy (49,50). The clinical success rate in this group was 90–95%, with a complication rate of 25–44%.
Comparative outcomes
A total of 12 publications assessed comparative outcomes for patients with AGC, including stenting versus surgery, surgery versus surgery, or surgery versus no surgery (see Table 4 and Figure 3) (51-62).
Stent versus surgery
Eight studies examined outcomes between stenting versus surgery, including endoscopic placement of SEMS versus stomach-partitioning gastrojejunostomy, partial gastrectomy with Roux-en-Y gastrojejunostomy, and gastrojejunostomy alone. Taken together, the studies demonstrated a faster return to oral intake with fewer complications and shorter index hospitalizations for patients undergoing stenting compared to surgical intervention however, the median symptom-free interval and median patency rate was longest in those undergoing palliative resection (54). Patients undergoing surgical intervention had complications, including delayed gastric emptying, pulmonary embolism, bleeding requiring reoperation, and wound infection. The rate of late adverse events was significantly higher in the stenting group (56).
Surgery versus surgery
Four studies examined outcomes between two types of surgical interventions (59-62). One study assessed outcomes following open versus laparoscopic gastrojejunostomy (59). The open group had a higher rate of postoperative delayed gastric emptying compared to the laparoscopic group. The median time to resumption of oral intake was 4 days after open surgery compared to 2 days after laparoscopic surgery (59). A separate study analyzed outcomes following non-curative intent gastrectomy versus gastrojejunostomy; in patients undergoing non-curative intent gastrectomy versus gastrojejunostomy, there was improvement in the GOOSS score in most of the patients with acceptable patency rates at the end of 90 days (60). The final study investigated gastric partitioning with gastrojejunostomy or Roux-en-Y versus gastrojejunostomy (61). In this study, oral tolerance of soft solids and low-residue or full diet were achieved by 93.3% of patients who had undergone gastric partitioning compared to 75.9% of patients who had undergone gastrojejunostomy (61). There were no differences in postoperative complications or surgical mortality between groups. Finally, one study examined differences between gastrectomy, exploration without resection, and no surgery (62). The authors showed that a R2 gastrectomy improved abdominal pain in 44% of patients and improved symptoms of nausea and vomiting in 40% of patients. This was significantly better than exploration without resection however the procedure was associated with more postoperative complications.
Ascites
Symptom description
Intraabdominal ascites causes a fullness or a tense feeling in the abdomen, depending on severity. Malignant and non-malignant ascites have similar symptom profiles, however, malignant ascites is often recalcitrant to interventions and reaccumulates quickly. In this section, ascites was graded by symptom experience (66), and by computed tomography (CT) as either none (undetectable by CT scanning), mild (localized in only the upper abdominal space or pelvis), moderate (neither mild nor massive), or massive (ascites filled the abdomen and pelvis) (67).
Treatment modalities
Two treatment modalities were used to address symptoms of malignant ascites for patients with AGC including HIPEC and intravenous chemotherapy alone (see Table 6 and Figure 4).
Table 6
| Category | Year | Title | Study design | N | Outcome | Intervention | Conclusions | Overall quality rating |
|---|---|---|---|---|---|---|---|---|
| HIPEC for ascites | 2014 | Hyperthermic intraperitoneal chemoperfusion in combined treatment of locally advanced and disseminated gastric cancer: results of a single-centre study (66) | Retrospective case-control study, single institution | 98 | Secondary outcome | Cytoreductive surgery in combination with HIPEC versus either cytoreductive surgery without HIPEC, palliative chemotherapy, or best supportive care | In the HIPEC subgroup, 20% of patients required post-operative paracentesis compared to 100% of patients in the control subgroup | Moderate |
| HIPEC for ascites | 2012 | Whole-body hyperthermia combined with hyperthermic intraperitoneal chemotherapy for the treatment of stage IV advanced gastric cancer (68) | Not specified | 26 | Secondary outcome | Two treatment sessions of combined therapy of whole-body hyperthermia and hyperthermic intraperitoneal chemo-perfusion versus oxaliplatin combined with 5-FU chemotherapy or Xeloda | The complete and partial remission rate of ascites was 70.6% in the intervention group and 33.3% in the control group. Karnofsky scores improved in the intervention group and were superior to the chemotherapy control group | Very Low |
| HIPEC for ascites | 2022 | Hyperthermic intraperitoneal chemotherapy plus intravenous chemotherapy of paclitaxel with or without sintilimab in gastric cancer: a comparative study (69) | Prospective randomized controlled trial, single institution | 120 | Secondary outcome | Cytoreductive surgery and HIPEC (HIPEC was performed 48 hours postoperatively, for 4 times in total on alternate days) plus intravenous chemotherapy of paclitaxel with or without sintilimab versus paclitaxel intravenous chemotherapy only | The objective remission rate of ascites in the study group was significantly higher than that in the control group. After treatment, significantly higher KPS scores were observed in the study group versus those of the control group | Low |
| Chemo for ascites | 2018 | First-line bolus 5-fluorouracil plus leucovorin for peritoneally disseminated gastric cancer with massive ascites or inadequate oral intake (67) | Retrospective case series, single institution | 30 | Secondary outcome | Intravenous 5-FU bolus plus leucovorin infusion on a 6 weeks on/2 weeks off schedule | 40% of the patients in the series had massive ascites at presentation (filled the abdomen and pelvis on CT imaging); improvement in ascites occurred in 39% of all patients presenting with ascites | Low |
| Chemo for ascites | 2012 | First-line fluorouracil-based chemotherapy for patients with severe peritoneal disseminated gastric cancer (70) | Retrospective case series, single institution | 92 | Primary outcome | 5-FU-based chemotherapy | 43% of the patients in the series had massive ascites; among the patients having assessable ascites, 27% showed an improvement in ascites | Very low |
AGC, advanced gastric cancer; HIPEC, hyperthermic intraperitoneal chemoperfusion; KPS, Karnofsky performance status; 5-FU, 5-fluorouracil; CT, computed tomography.
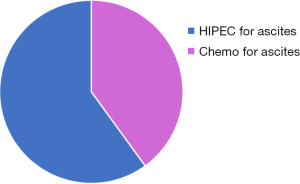
HIPEC for ascites
Three studies assessed HIPEC for the treatment of ascites in AGC and each study administered the HIPEC differently (66,68,69). Yarema et al. administered HIPEC intraoperatively following aggressive cytoreduction and found that 20% of patients required post-operative paracentesis compared to 100% of patients in the control subgroup (66). Zhao et al. (68) administered whole-body hyperthermia without cytoreduction in conjunction with intraperitoneal chemo-perfusion over two treatments and demonstrated a complete and partial remission rate of ascites of 70.6% in the intervention group compared to 33.3% in the control group. Finally, Zhang et al. administered HIPEC 48 hours postoperatively, for a total of 4 times on alternate days, and found that the objective remission rate of ascites in the study group was significantly higher than that in the control group (69).
Chemotherapy for ascites
Two studies evaluated the use of fluorouracil-based chemotherapy in the treatment of ascites for AGC (67,70). In these studies, improvement in ascites occurred in 27-39% of all patients who presented with ascites.
Comparative outcomes
There were no published studies regarding comparative outcomes for the treatment of ascites secondary to AGC during the timeframe of 2010–2022.
QoL
Description
Studies in this group evaluated QoL in a spectrum of patient populations, including those receiving chemotherapy, radiotherapy, supplemental nutrition, and procedural interventions including surgery. Several different QoL metrics were used to characterize symptoms, the overall impact of AGC, and its related interventions (see Table 7).
Table 7
| Gastric Outlet Obstruction Score (GOOS) |
| Dysphagia Outcome and Severity Scale (DOSS) |
| CTCAE grade for UGIB |
| Functional Assessment of Cancer Therapy: Gastric Questionnaire |
| EORTC QLQ-C30 |
| EORTC QLQ-STO22; gastric-specific module |
| EORTC QLQ-FA12 |
| Euro QoL Five Dimensions Questionnaire (EQ-5D) |
| Palliative Prognostic Index (PPI) |
| Support Team Assessment Schedule (STAS) |
| Integrated Patient Outcome Scale (IPOS) |
| Trial Outcome Index (TOI) |
| Generic Quality of Life Inventory-74 Scale (GQOLI-74) |
| Hamilton Anxiety Scale (HAMA) |
| Hamilton Depression Scale (HAMD) |
| Karnofsky Performance Scale (KPS) |
| Short Form Health Survey Questionnaire (SF-36) |
QoL, quality of life; AGC, advanced gastric cancer; UGIB, upper gastrointestinal bleeding; CTCAE, Common Terminology Criteria for Adverse Events; EORTC, European Organization for Research and Treatment of Cancer; QLQ, Quality of Life Questionnaire.
Treatment modalities
A total of 15 studies assess varying aspects of QoL. Five studies focused on QoL while receiving systemic therapies (71-75), three studies assessed QoL after surgical interventions (76-78), one study examined QoL after percutaneous liver ablation (79), two studies considered QoL during radiation treatments (80,81), two studies assessed QoL with nutritional interventions (82,83), two studies evaluated QoL in the last 6 months of life with or without the support of hospice services (84,85), and the last study examined the effects of low-frequency rotary magnetic fields on patients with symptomatic AGC (see Table 8 and Figure 5) (86). All studies were quantitative, as the only study reporting on the qualitative experiences of patients with gastric cancer did not specify that the patients in that study had AGC (87).
Table 8
| Category | Year | Title | Study design | N | Outcome | Study type | Intervention | Conclusion | Overall quality rating |
|---|---|---|---|---|---|---|---|---|---|
| QoL during systemic therapy for AGC | 2019 | Treatment patterns and changes in quality of life during first-line palliative chemotherapy in Korean patients with advanced gastric cancer (71) | Prospective case series, multi-institutional | 527 | Secondary outcome | Quantitative | First-line palliative chemotherapy (mainly 5-FU-based chemotherapy plus platinum) | Small positive changes were observed in physical functioning, role functioning, cognitive functioning, global health status, pain, dyspnea, insomnia, appetite loss, constipation, reflux symptoms, dry mouth, taste, body image, and hair loss. Emotional functioning, social functioning, and global health status/QoL showed improvements with statistical significance | High |
| QoL during systemic therapy for AGC | 2017 | Quality of life with biweekly docetaxel and capecitabine in advanced gastro-oesophageal cancer (72) | Non-randomized clinical trial, multi-institutional | 53 | Primary outcome | Quantitative | Biweekly docetaxel with capecitabine | No deterioration in global health status was found. Social functioning scores improved, and eating difficulties and pain were alleviated during treatment | Moderate |
| QoL during systemic therapy for AGC | 2021 | Clinical impact of oral intake in second-line or third-line chemotherapy for 589 patients with advanced gastric cancer: a retrospective cohort study (73) | Retrospective case series, single institution | 589 | Primary outcome | Quantitative | Later-line chemotherapy | As disease progressed during first-line, second-line, and third-line chemotherapy, 78.3%, 53.3%, and 30.4% of patients exhibited sufficient oral intake. Fourth-line chemotherapy was initiated for 22.2% of patients, with 20.0% exhibiting sufficient oral intake. Factors correlated to deterioration in oral intake during second-line chemotherapy were poor ECOG performance status, moderate or severe ascites, peritoneal metastasis, and prior palliative surgery | Moderate |
| QoL during systemic therapy for AGC | 2020 | Effects of S-1 combined with palliative care on immune function and quality of life of patients with advanced stomach cancer (74) | Not specified | 168 | Secondary outcome | Quantitative | S-1 (a novel oral dihydropyrimidine dehydrogenase inhibitor) alone versus combined with palliative care | QoL improvement rate was significantly higher in patients receiving palliative care compared to those not receiving palliative care | Very low |
| QoL during systemic therapy for AGC | 2019 | Evaluation of efficacy and safety of apatinib treatment in advanced gastric cancer (75) | Non-randomized clinical trial, single institution | 24 | Secondary outcome | Quantitative | Apatinib daily dose of 500 mg for 4 weeks per cycle until disease progression or intolerable toxicity | The QoL score was elevated after three treatment cycles but it was not statistically significant | Moderate |
| QoL after surgery | 2019 | Pressurized intraperitoneal aerosol chemotherapy with low-dose cisplatin and doxorubicin (PIPAC C/D) in patients with gastric cancer and peritoneal metastasis: a phase II study (76) | Non-randomized clinical trial, single institution | 25 | Secondary outcome | Quantitative | Three courses of PIPAC with cisplatin and doxorubicin every 6 weeks | Changes in the QLQ-C30 scores were small and not significant | Moderate |
| QoL after surgery | 2012 | The clinical value of non-curative resection followed by chemotherapy for incurable gastric cancer (77) | Retrospective case series, single institution | 178 | Secondary outcome | Quantitative | Non-curative gastric resection | For symptomatic patients, the symptom-relief period was 8.6 months on average | Low |
| QoL after surgery | 2012 | Non-curative gastrectomy for metastatic gastric cancer: rationale and long-term outcome in multicenter settings (78) | Retrospective case series with a prospective component, multi-institutional | 140 | Secondary outcome | Quantitative | Non-curative gastric resection | A gradual impairment in QoL parameters were found over 12 months after non-curative resections but changes did not reach statistical significance | Moderate |
| QoL after ablation | 2018 | CT-guided percutaneous cryoablation for palliative therapy of gastric cancer liver metastases (79) | Retrospective case series, single institution | 19 | Secondary outcome | Quantitative | Percutaneous cryoablation of liver metastases | The mean scores for physical well-being and functional well-being increased while the scores for social and emotional well-being remained unchanged. The total QoL score improved over the study period and was statistically significant | Moderate |
| QoL during radiation therapy | 2010 | Consideration of the role of radiotherapy for abdominal lymph node metastases in patients with recurrent gastric cancer (81) | Retrospective cohort study, single institution | 79 | Secondary outcome | Quantitative | Palliative radiotherapy | Clinical symptoms were relieved in 90.5% after completing radiation | Low |
| QoL with nutrition | 2018 | Feasibility of intravenous iron isomaltoside to improve anemia and quality of life during palliative chemotherapy for esophagogastric adenocarcinoma (82) | Randomized-controlled trial, multi-instutional | 27 | Secondary outcome | Quantitative | Standard of care or single dose of IVI before chemotherapy | Intravenous iron improved QoL with physical well-being, emotional well-being, anemia-specific QoL, trial outcome index, and total scores all exceeding minimum clinically important difference. No improvement was seen with standard care | Moderate |
| QoL with nutrition | 2021 | Supplemental home parenteral nutrition improved nutrition status with comparable quality of life in malnourished unresectable/metastatic gastric cancer receiving salvage chemotherapy (83) | Non-randomized clinical trial, single institution | 25 | Secondary outcome | Quantitative | Home parenteral nutrition | Global QoL scores were maintained and comparable with those of the control group | High |
| QoL during last 6 months of life | 2021 | Patient-reported symptoms in metastatic gastric cancer patients in the last 6 months of life (84) | Retrospective cohort study, multi-institutional | 788 | Primary outcome | Quantitative | None; this was a descriptive study of symptom trajectories and risk factors for increased symptom severity for patients with AGC | The highest prevalence of moderate-to-severe scores was observed for tiredness and lack of appetite. The overall rates of moderate-to-severe symptom scores rose as patients neared death, with a prevalence of moderate-to severe scores 50% or greater for all symptoms except nausea in the final month of life | Very low |
| QoL on hospice | 2021 | Impact of pain care and hospice care on quality of life in patients with advanced gastric cancer (85) | Randomized-controlled trial, single institution | 136 | Primary outcome | Quantitative | Hospice care and pain interventions | The intervention group had higher reported improvements in the domains of physiological function, psychological function, emotional function, social function, and mental health compared to the control group | Very low |
| Other | 2018 | Effect of low-frequency rotary magnetic fields on advanced gastric cancer: survival and palliation of general symptoms (86) | Non-randomized clinical trial, single institution | 21 | Primary outcome | Quantitative | Magnetic fields | Improved abdominal pain in 42.9%, nausea/vomiting in 19.0%m, weight loss in 52.4%, ongoing blood loss in 9.5%, physical strength in 23.8), and sleep quality in 19.0% | High |
QoL, quality of life; AGC, advanced gastric cancer; 5-FU, 5-fluorouracil; ECOG, Eastern Cooperative Oncology Group; PIPAC, pressurized intraperitoneal aerosol chemotherapy; QLQ-C30, Quality of Life Questionnaire Core 30; IVI, intravenous iron isomaltoside.
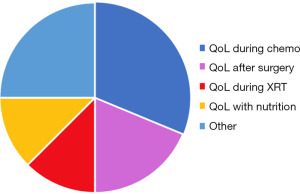
QoL during systemic therapy
Systemic therapies in this group of reviews spans first-line to last-line chemotherapeutic options, oral fluoropyrimidines, S-1, and tyrosine-kinase inhibitors (i.e., apatinib). Investigators found that patients taking these agents showed no deterioration in global health status and had improved social functioning scores. Small changes were observed in physical functioning, pain, dyspnea, insomnia, appetite loss, constipation, reflux symptoms, dry mouth, taste, body image, and hair loss, cognitive functioning, and global health status, as well as the ability to carry out social roles (such as parenting, being a spouse, etc.). Social functioning, emotional functioning, and global health status/QoL showed improvements that gained statistical significance. Patients on fourth-line treatments demonstrated insufficient oral intake as compared to patients on first-, second-, and third-line treatments, reflecting more severe/progressive disease in this population of patients.
QoL after surgery
Additional QoL outcomes after surgery are discussed above in the obstruction section, however, from a global perspective, for patients undergoing surgical intervention in the absence of symptomatic obstruction, overall QoL was not as drastically improved. Two of the three studies showed insignificant differences in QoL (76,78), and one study documented an average 8.6 months of symptom relief after surgical intervention (77).
QoL after ablation
One study assessed QoL after percutaneous liver ablation for metastatic gastric cancer. The mean scores for physical well-being and functional well-being increased while the scores for social and emotional well-being remained unchanged. The total QoL score was statistically significant. Most patients experienced minor limitations after the procedure, including pain at the percutaneous puncture site, fever, transient liver damage, and pleural effusion, which all recovered spontaneously or as a result of timely supportive treatment.
QoL during radiation therapy
One retrospective study reported general QoL improvements after the completion of palliative-intent radiation (81). The study showed symptomatic improvement in 90.5% of patients.
QoL with nutritional intervention
Two studies addressed nutritional interventions for patients with AGC, namely intravenous iron administration and supplemental home parenteral nutrition (82,83). Patients receiving intravenous iron demonstrated improved QoL with physical well-being, emotional well-being, and anemia-specific QoL. The study of home parental nutrition revealed that QoL scores were maintained and statistically equivalent to those in the control group.
QoL in the last 6 months of life
One study was a descriptive study of symptom for patients with AGC. The authors found that tiredness and lack of appetite were the two most intrusive symptoms for this patient population. The overall rates of moderate-to-severe symptom scores increased as patients neared death, with a prevalence of moderate-to-severe scores 50% or greater for all symptoms except nausea in the final month of life.
Other
A final study assessed the effects of low-frequency rotary magnetic fields on AGC and demonstrated improved abdominal pain, nausea, vomiting, and weight loss (86).
Comparative outcomes
Two studies in this category were comparative studies. The first, discussed above, evaluated standard of care versus single dose of intravenous iron before chemotherapy, and found that the group randomized to intravenous iron showed improvements in physical well-being, emotional well-being, and anemia-specific QoL (82). A final study assessed QoL for patients with and without hospice support services (85).
QoL with or without the support of hospice services
In this study, the intervention group (patients receiving hospice support services) had higher reported improvements in the domains of physiological function, psychological function, emotional function, social function, and mental health compared to the control group.
Palliative care consultation and advanced care planning
Only one study assessed outcomes for patients with AGC who had received palliative care consultation (88). This study was a prospective, multicenter study, randomized trial of patients who received either standard cancer care or standard cancer care plus early palliative care specialty consultation and was of moderate quality. The primary outcome was a change in QoL, as measured by the Functional Assessment of Cancer Therapy-Gastric questionnaire 12 weeks after randomization. The results demonstrated a slight, but not statistically significant, benefit of early palliative care. No studies were published on advanced care planning specific to the AGC patient population.
Quality of included studies and risk for bias
Of the total 66 included studies, eight were rated high quality, 38 were rated moderate quality, and 20 studies were rated low or very low quality, indicating a high likelihood of bias. Most studies answered a specific study question, clearly described the patient population and the intervention studied, and used validated outcomes measures that were applied consistently. However, the large majority of studies included were retrospective in nature and had small sample sizes (often N<50). Not all studies accounted for possible confounders in their design and statistical analysis.
Discussion
This study reviewed the palliative interventions currently available for patients with AGC with a focus on symptom management and QoL in accordance with the WHO’s definition of a palliative approach (7). Palliative interventions for symptoms related to bleeding and obstruction were well characterized in the literature though the primary outcomes were almost exclusively focused on resolution of the acute bleeding. For instance, in the bleeding category, all studies except one exclusively defined success of the primary intervention as resolution of bleeding. Only one study included the broader symptom profile of shortness of breath, pain, and distress, and no studies assessed the psychosocial or emotional impact of bleeding. No studies assessed shared decision-making to help patients and providers consider outcomes and alternatives (i.e., radiation versus endoscopy versus surgical intervention versus hospice). No publications examined the inconvenience of daily radiation therapies or the impact it had on the patient’s overall QoL. Additionally, radiation and chemotherapy delivered for bleeding have physiologic side effects including fatigue, nausea, and vomiting and these side effects were unaccounted for in the present studies which predominantly categorize success as the discontinuation of hemorrhage.
Similar trends were identified in the publications outlining interventions for patients with obstructive symptoms. The primary outcome in nearly all studies was resumption of oral intake, length of hospital stay, and the need for re-intervention. Only one study evaluated global QoL domains, and no studies performed qualitative assessments of the patient’s experience with obstruction and any required interventions. As above, no studies assessed shared decision-making to help patients and providers consider outcomes and alternatives (i.e., endoscopic stenting versus surgical intervention versus hospice), and no publications examined the impact that obstruction had on patients’ psychosocial QoL. Similar patterns were found for studies examining ascites.
The various interventions that studied QoL as a primary or secondary outcome measure did tend to capture a broader picture of the patient’s overall QoL, including emotional and social functioning in addition to physical and cognitive functioning, global health status, pain, dyspnea, insomnia, appetite loss, constipation, reflux symptoms, dry mouth, taste, body image, and hair loss. However, each of these studies was quantitative, with a lack of rich descriptions of the patient experience. The majority of the QoL outcomes were secondary outcome measures and thusly not as well characterized as the lauded outcome measures of overall survival, technical success, and tumor response as measured by imaging, to name a few.
During the process of reviewing the literature, we identified studies examining the use of endoscopically placed topical hemostatic agents which prevent tumor bleeding by providing immediate hemostasis. Unfortunately, no studies of these agents were performed in populations comprising >50% AGC patients. We also noted papers that described endoscopic ultrasound-guided gastrojejunostomy, but unfortunately, none of the publications comprised of >50% AGC patients and thus had to be excluded.
Our work builds on a review by Mahar et al., published in 2012 (6). The authors argued that relief of symptoms should be the primary focus of palliative treatment. Despite improvements in specific areas over the last decade there is still significant work to be done to characterize the spectrum of symptoms associated with AGC and its treatment options. We agree with the authors that there continues to be a need for more prospectively designed studies in this area of research, and we believe that qualitative and mixed-methods studies are required to better characterize the patient experience. This information should be used to guide shared decision-making and allow for a more comprehensive and nuanced understanding of the risks, benefits, and alternatives associated with each palliative-focused intervention.
Limitations
Like all systematic reviews, our study has limitations including potentially missed publications despite a comprehensive search of multiple databases and citation searching with manual review.
Conclusions
This study reviewed the palliative interventions currently available for patients with AGC, with a focus on symptom management and QoL in accordance with the WHO’s definition of a palliative approach (7). Palliative interventions for symptoms related to bleeding and obstruction were well characterized in the literature, as were the interventions for the symptomatic burden of ascites, though to a lesser extent. There was a significant amount of heterogeneity in the studies that assessed QoL. Importantly, no studies were identified that described advanced care planning in this patient population. Prospective research with credible and comprehensive outcome measures related to symptom management and QoL as well as research exploring the psychosocial and spiritual domains of care in AGC is required.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Adam Yopp) for the series “Multimodal Management of Gastric and Gastroesophageal Cancers” published in Chinese Clinical Oncology. The article has undergone external peer review.
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://cco.amegroups.com/article/view/10.21037/cco-22-102/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://cco.amegroups.com/article/view/10.21037/cco-22-102/coif). The series “Multimodal Management of Gastric and Gastroesophageal Cancers” was commissioned by the editorial office without any funding or sponsorship. KK attended an industry-sponsored education event through the AHPBA (Americas hepatobiliary Association) in conjunction with his role as a clinical fellow in surgical oncology and hepatobiliary surgery in the United States. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Thrift AP, El-Serag HB. Burden of Gastric Cancer. Clin Gastroenterol Hepatol 2020;18:534-42. [Crossref] [PubMed]
- Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2018;68:394-424. [Crossref] [PubMed]
- Johnston FM, Beckman M. Updates on Management of Gastric Cancer. Curr Oncol Rep 2019;21:67. [Crossref] [PubMed]
- Eeson G, Brar SS, Coburn NG. Gastric Adenocarcinoma. In: Wright F, Escallon J, Cukier M, et al. editors. Surgical Oncology Manual. 2nd ed. Cham: Springer 2016:137-48.
- Harada K, Zhao M, Shanbhag N, et al. Palliative care for advanced gastric cancer. Expert Rev Anticancer Ther 2020;20:575-80. [Crossref] [PubMed]
- Mahar AL, Coburn NG, Singh S, et al. A systematic review of surgery for non-curative gastric cancer. Gastric Cancer 2012;15:S125-37. [Crossref] [PubMed]
- Sepúlveda C, Marlin A, Yoshida T, et al. Palliative Care: the World Health Organization's global perspective. J Pain Symptom Manage 2002;24:91-6. [Crossref] [PubMed]
- Seaman JB, Lakin JR, Anderson E, et al. Interdisciplinary or Interprofessional: Why Terminology in Teamwork Matters to Hospice and Palliative Care. J Palliat Med 2020;23:1157-8. [Crossref] [PubMed]
- Covidence systematic review software. Melbourne: Veritas Health Innovation. Available online: https://www.covidence.org/
- Ma LL, Wang YY, Yang ZH, et al. Methodological quality (risk of bias) assessment tools for primary and secondary medical studies: what are they and which is better? Mil Med Res 2020;7:7. [Crossref] [PubMed]
- National Heart, Lung, and Blood Home. Study Quality Assessment Tools. [cited 2022 Nov 29]. Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools
- Critical Appraisal Skills Programme. CASP Checklists. [cited 2022 Nov 29]. Available online: https://casp-uk.net/casp-tools-checklists/
- Cochrane Methods Bias. ROBINS-I. [cited 2022 Nov 29]. Available online: https://methods.cochrane.org/bias/risk-bias-non-randomized-studies-interventions
- Higgins JPT, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928. [Crossref] [PubMed]
- Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372: [PubMed]
- Choi CY. Palliative haemostatic radiotherapy for advanced cancer of the stomach. J Pain Manag 2012;5:53.
- Asakura H, Hashimoto T, Harada H, et al. Palliative radiotherapy for bleeding from advanced gastric cancer: is a schedule of 30 Gy in 10 fractions adequate? J Cancer Res Clin Oncol 2011;137:125-30. [Crossref] [PubMed]
- Hiramoto S, Kikuchi A, Tetsuso H, et al. Efficacy of palliative radiotherapy and chemo-radiotherapy for unresectable gastric cancer demonstrating bleeding and obstruction. Int J Clin Oncol 2018;23:1090-4. [Crossref] [PubMed]
- Kawabata H, Fujii T, Yamamoto T, et al. Palliative Radiotherapy for Bleeding from Unresectable Gastric Cancer Using Three-Dimensional Conformal Technique. Biomedicines 2022;10:1394. [Crossref] [PubMed]
- Chaw CL, Niblock PG, Chaw CS, et al. The role of palliative radiotherapy for haemostasis in unresectable gastric cancer: a single-institution experience. Ecancermedicalscience 2014;8:384. [PubMed]
- Lee J, Byun HK, Koom WS, et al. Efficacy of radiotherapy for gastric bleeding associated with advanced gastric cancer. Radiat Oncol 2021;16:161. [Crossref] [PubMed]
- Mitsuhashi N, Ikeda H, Nemoto Y, et al. Hemostatic Effect of Palliative Radiation Therapy in Preventing Blood Transfusions from Bleeding Occurring within Advanced Gastric Cancer. Palliat Med Rep 2021;2:355-64. [Crossref] [PubMed]
- Lee YH, Lee JW, Jang HS. Palliative external beam radiotherapy for the treatment of tumor bleeding in inoperable advanced gastric cancer. BMC Cancer 2017;17:541. Erratum in: BMC Cancer 2018;18:232. [Crossref] [PubMed]
- Sugita H, Sakuramoto S, Mihara Y, et al. Verification of the Utility of Palliative Radiotherapy for Hemostasis of Gastric Cancer Bleeding: a Case Control Study. J Gastrointest Cancer 2022;53:420-6. [Crossref] [PubMed]
- Takeda K, Sakayauchi T, Kubozono M, et al. Palliative radiotherapy for gastric cancer bleeding: a multi-institutional retrospective study. BMC Palliat Care 2022;21:52. [Crossref] [PubMed]
- Tey J, Choo BA, Leong CN, et al. Clinical outcome of palliative radiotherapy for locally advanced symptomatic gastric cancer in the modern era. Medicine (Baltimore) 2014;93:e118. [Crossref] [PubMed]
- Tey J, Zheng H, Soon YY, et al. Palliative radiotherapy in symptomatic locally advanced gastric cancer: A phase II trial. Cancer Med 2019;8:1447-58. [Crossref] [PubMed]
- Yu J. Role of palliative radiotherapy in bleeding control in patients with unresectable advanced gastric cancer. BMC Cancer 2021;21:413. [Crossref] [PubMed]
- Kondoh C, Shitara K, Nomura M, et al. Efficacy of palliative radiotherapy for gastric bleeding in patients with unresectable advanced gastric cancer: a retrospective cohort study. BMC Palliat Care 2015;14:37. [Crossref] [PubMed]
- Kawamoto T, Saito T, Kosugi T, et al. Temporal Profiles of Symptom Scores After Palliative Radiotherapy for Bleeding Gastric Cancer With Adjustment for the Palliative Prognostic Index: An Exploratory Analysis of a Multicentre Prospective Observational Study (JROSG 17-3). Clin Oncol (R Coll Radiol) 2022;34:e505-14. [Crossref] [PubMed]
- Kawabata H, Uno K, Yasuda K, et al. Experience of Low-Dose, Short-Course Palliative Radiotherapy for Bleeding from Unresectable Gastric Cancer. J Palliat Med 2017;20:177-80. [Crossref] [PubMed]
- Park S, Shin JH, Gwon DI, et al. Transcatheter Arterial Embolization for Gastrointestinal Bleeding Associated with Gastric Carcinoma: Prognostic Factors Predicting Successful Hemostasis and Survival. J Vasc Interv Radiol 2017;28:1012-21. [Crossref] [PubMed]
- Cho SB, Hur S, Kim HC, et al. Transcatheter arterial embolization for advanced gastric cancer bleeding: A single-center experience with 58 patients. Medicine (Baltimore) 2020;99:e19630. [Crossref] [PubMed]
- Kim YI, Choi IJ, Cho SJ, et al. Outcome of endoscopic therapy for cancer bleeding in patients with unresectable gastric cancer. J Gastroenterol Hepatol 2013;28:1489-95. [Crossref] [PubMed]
- Koh KH, Kim K, Kwon DH, et al. The successful endoscopic hemostasis factors in bleeding from advanced gastric cancer. Gastric Cancer 2013;16:397-403. [Crossref] [PubMed]
- Biswas S, Acharyya S, Roy P, et al. Efficacy of Chronomodulated Chemotherapy for Palliation of Hematemesis in Inoperable Gastric Cancer: A Single-Institutional Retrospective Study. Indian J Palliat Care 2020;26:342-7. [Crossref] [PubMed]
- Kim YI, Kim MJ, Park SR, et al. Effect of a Proton Pump Inhibitor on Tumor Bleeding Prevention in Unresectable Gastric Cancer Patients: a Double-Blind, Randomized, Placebo-Controlled Trial. J Gastric Cancer 2017;17:120-31. [Crossref] [PubMed]
- Yagi S, Ida S, Namikawa K, et al. Clinical outcomes of palliative treatment for gastric bleeding from incurable gastric cancer. Surg Today 2022; Epub ahead of print. [Crossref] [PubMed]
- Tey J, Soon YY, Koh WY, et al. Palliative radiotherapy for gastric cancer: a systematic review and meta-analysis. Oncotarget 2017;8:25797-805. [Crossref] [PubMed]
- Forrest JA, Finlayson ND, Shearman DJ. Endoscopy in gastrointestinal bleeding. Lancet 1974;2:394-7. [Crossref] [PubMed]
- Endo S, Takiguchi S, Miyazaki Y, et al. Efficacy of endoscopic gastroduodenal stenting for gastric outlet obstruction due to unresectable advanced gastric cancer: a prospective multicenter study. J Surg Oncol 2014;109:208-12. [Crossref] [PubMed]
- Lye TJ, Goh YC, Eng AK, et al. Endoscopic self-expandable metallic stenting for palliation of malignant gastric outlet obstruction in Southeast Asia. ANZ J Surg 2016;86:464-8. [Crossref] [PubMed]
- Caglar E, Dobrucali A. Self-expandable metallic stent placement in the palliative treatment of malignant obstruction of gastric outlet and duodenum. Clin Endosc 2013;46:59-64. [Crossref] [PubMed]
- Shi D, Bao YS, Liu YP. Individualization of metal stents for management of gastric outlet obstruction caused by distal stomach cancer: a prospective study. Gastrointest Endosc 2013;78:277-84. [Crossref] [PubMed]
- Kim DY, Moon HS, Kwon IS, et al. Self-expandable metal stent of esophagogastric junction versus pyloric area obstruction in advanced gastric cancer patients: Retrospective, comparative, single-center study. Medicine (Baltimore) 2020;99:e21621. [Crossref] [PubMed]
- Fernández-Moreno MC, Martí-Obiol R, López F, et al. Modified Devine Exclusion for Unresectable Distal Gastric Cancer in Symptomatic Patients. Case Rep Gastroenterol 2017;11:9-16. [Crossref] [PubMed]
- Ito Y, Fujitani K, Sakamaki K, et al. QOL assessment after palliative surgery for malignant bowel obstruction caused by peritoneal dissemination of gastric cancer: a prospective multicenter observational study. Gastric Cancer 2021;24:1131-9. [Crossref] [PubMed]
- Fujitani K, Yamada M, Hirao M, et al. Optimal indications of surgical palliation for incurable advanced gastric cancer presenting with malignant gastrointestinal obstruction. Gastric Cancer 2011;14:353-9. [Crossref] [PubMed]
- Kim J, Choi IJ, Kim CG, et al. Self-expandable metallic stent placement for malignant obstruction in patients with locally recurrent gastric cancer. Surg Endosc 2011;25:1505-13. [Crossref] [PubMed]
- Park JH, Song HY, Kim SH, et al. Metallic stent placement in patients with recurrent malignant obstruction in the surgically altered stomach. Ann Surg Oncol 2014;21:2036-43. [Crossref] [PubMed]
- Fiori E, Crocetti D, Sapienza P, et al. Palliative Surgery or Metallic Stent Positioning for Advanced Gastric Cancer: Differences in QOL. Medicina (Kaunas) 2021;57:428. [Crossref] [PubMed]
- Alonso-Lárraga JO, Alvaro-Villegas JC, Sobrino-Cossío S, et al. Self-expanding metal stents versus antrectomy for the palliative treatment of obstructive adenocarcinoma of the gastric antrum. Rev Esp Enferm Dig 2012;104:185-9. [Crossref] [PubMed]
- Haga Y, Hiki N, Kinoshita T, et al. Treatment option of endoscopic stent insertion or gastrojejunostomy for gastric outlet obstruction due to gastric cancer: a propensity score-matched analysis. Gastric Cancer 2020;23:667-76. [Crossref] [PubMed]
- Keränen I, Kylänpää L, Udd M, et al. Gastric outlet obstruction in gastric cancer: a comparison of three palliative methods. J Surg Oncol 2013;108:537-41. [Crossref] [PubMed]
- Fiori E, Sterpetti AV, De Cesare A, et al. Factors Leading to Improved Results for Endoscopic Stenting for Metastatic Antropyloric Adenocarcinoma. A Comparison with Gastrojejunostomy. J Gastrointest Surg 2016;20:1802-6. [Crossref] [PubMed]
- No JH, Kim SW, Lim CH, et al. Long-term outcome of palliative therapy for gastric outlet obstruction caused by unresectable gastric cancer in patients with good performance status: endoscopic stenting versus surgery. Gastrointest Endosc 2013;78:55-62. [Crossref] [PubMed]
- Jang SH, Lee H, Min BH, et al. Palliative gastrojejunostomy versus endoscopic stent placement for gastric outlet obstruction in patients with unresectable gastric cancer: a propensity score-matched analysis. Surg Endosc 2017;31:4217-23. [Crossref] [PubMed]
- Park JH, Song HY, Yun SC, et al. Gastroduodenal stent placement versus surgical gastrojejunostomy for the palliation of gastric outlet obstructions in patients with unresectable gastric cancer: a propensity score-matched analysis. Eur Radiol 2016;26:2436-45. [Crossref] [PubMed]
- Ojima T, Nakamori M, Nakamura M, et al. Laparoscopic Gastrojejunostomy for Patients with Unresectable Gastric Cancer with Gastric Outlet Obstruction. J Gastrointest Surg 2017;21:1220-5. [Crossref] [PubMed]
- Purkayastha J, Bannoth S, Kalita D, et al. A Study of Clinical Presentation and Management of Malignant Gastric Outlet Obstruction (Northeast India-Based Single-Centre Experience). Indian J Surg Oncol 2019;10:649-53. [Crossref] [PubMed]
- Ramos MFKP, Barchi LC, de Oliveira RJ, et al. Gastric partitioning for the treatment of malignant gastric outlet obstruction. World J Gastrointest Oncol 2019;11:1161-71. [Crossref] [PubMed]
- Collins A, Hatzaras I, Schmidt C, et al. Gastrectomy in advanced gastric cancer effectively palliates symptoms and may improve survival in select patients. J Gastrointest Surg 2014;18:491-6. [Crossref] [PubMed]
- Piesman M, Kozarek RA, Brandabur JJ, et al. Improved oral intake after palliative duodenal stenting for malignant obstruction: a prospective multicenter clinical trial. Am J Gastroenterol 2009;104:2404-11. [Crossref] [PubMed]
- Adler DG, Baron TH. Endoscopic palliation of malignant gastric outlet obstruction using self-expanding metal stents: experience in 36 patients. Am J Gastroenterol 2002;97:72-8. [Crossref] [PubMed]
- Troncone E, Fugazza A, Cappello A, et al. Malignant gastric outlet obstruction: Which is the best therapeutic option? World J Gastroenterol 2020;26:1847-60. [Crossref] [PubMed]
- Yarema RR, Ohorchak MA, Zubarev GP, et al. Hyperthermic intraperitoneal chemoperfusion in combined treatment of locally advanced and disseminated gastric cancer: results of a single-centre retrospective study. Int J Hyperthermia 2014;30:159-65. [Crossref] [PubMed]
- Hara H, Kadowaki S, Asayama M, et al. First-line bolus 5-fluorouracil plus leucovorin for peritoneally disseminated gastric cancer with massive ascites or inadequate oral intake. Int J Clin Oncol 2018;23:275-80. [Crossref] [PubMed]
- Zhao C, Dai C, Chen X. Whole-body hyperthermia combined with hyperthermic intraperitoneal chemotherapy for the treatment of stage IV advanced gastric cancer. Int J Hyperthermia 2012;28:735-41. [Crossref] [PubMed]
- Zhang Z, Ning MY, Han D, et al. Hyperthermic Intraperitoneal Chemotherapy plus Intravenous Chemotherapy of Paclitaxel with or without Sintilimab in Gastric Cancer: A Comparative Study. J Oncol 2022;2022:3054485. [Crossref] [PubMed]
- Iwasa S, Nakajima TE, Nakamura K, et al. First-line fluorouracil-based chemotherapy for patients with severe peritoneal disseminated gastric cancer. Gastric Cancer 2012;15:21-6. [Crossref] [PubMed]
- Kim JW, Kim JG, Kang BW, et al. Treatment Patterns and Changes in Quality of Life during First-Line Palliative Chemotherapy in Korean Patients with Advanced Gastric Cancer. Cancer Res Treat 2019;51:223-39. [Crossref] [PubMed]
- Korkeila EA, Salminen T, Kallio R, et al. Quality of life with biweekly docetaxel and capecitabine in advanced gastro-oesophageal cancer. Support Care Cancer 2017;25:2771-7. [Crossref] [PubMed]
- Ogata T, Narita Y, Kumanishi R, et al. Clinical Impact of Oral Intake in Second-line or Third-line Chemotherapy for 589 Patients With Advanced Gastric Cancer: A Retrospective Cohort Study. Am J Clin Oncol 2021;44:388-94. [Crossref] [PubMed]
- Wang Y, Li G. Effects of S-1 combined with palliative care on immune function and quality of life of patients with advanced stomach cancer. Oncol Lett 2020;20:2021-7. [Crossref] [PubMed]
- Yang Y, Wu X, Li F, et al. Evaluation of efficacy and safety of apatinib treatment in advanced gastric cancer. J Cancer Res Ther 2019;15:365-9. [PubMed]
- Struller F, Horvath P, Solass W, et al. Pressurized intraperitoneal aerosol chemotherapy with low-dose cisplatin and doxorubicin (PIPAC C/D) in patients with gastric cancer and peritoneal metastasis: a phase II study. Ther Adv Med Oncol 2019;11:1758835919846402. [Crossref] [PubMed]
- Ko KJ, Shim JH, Yoo HM, et al. The clinical value of non-curative resection followed by chemotherapy for incurable gastric cancer. World J Surg 2012;36:1800-5. [Crossref] [PubMed]
- Kulig P, Sierzega M, Kowalczyk T, et al. Non-curative gastrectomy for metastatic gastric cancer: rationale and long-term outcome in multicenter settings. Eur J Surg Oncol 2012;38:490-6. [Crossref] [PubMed]
- Chang X, Wang Y, Yu HP, et al. CT-guided percutaneous cryoablation for palliative therapy of gastric cancer liver metastases. Cryobiology 2018;82:43-8. [Crossref] [PubMed]
- Yamaguchi S, Ohguri T, Matsuki Y, et al. Palliative radiotherapy in patients with a poor performance status: the palliative effect is correlated with prolongation of the survival time. Radiat Oncol 2013;8:166. [Crossref] [PubMed]
- Sun J, Sun YH, Zeng ZC, et al. Consideration of the role of radiotherapy for abdominal lymph node metastases in patients with recurrent gastric cancer. Int J Radiat Oncol Biol Phys 2010;77:384-91. [Crossref] [PubMed]
- Ng O, Keeler B, Simpson JA, et al. Feasibility of Intravenous Iron Isomaltoside to Improve Anemia and Quality of Life During Palliative Chemotherapy for Esophagogastric Adenocarcinoma. Nutr Cancer 2018;70:1106-17. [Crossref] [PubMed]
- Ma CJ, Huang CW, Yeh YS, et al. Supplemental home parenteral nutrition improved nutrition status with comparable quality of life in malnourished unresectable/metastatic gastric cancer receiving salvage chemotherapy. Support Care Cancer 2021;29:1977-88. [Crossref] [PubMed]
- Bubis LD, Delibasic V, Davis LE, et al. Patient-reported symptoms in metastatic gastric cancer patients in the last 6 months of life. Support Care Cancer 2021;29:515-24. [Crossref] [PubMed]
- Ma X, Sun S, Zhao Y, et al. Impact of pain care and hospice care on quality of life in patients with advanced gastric cancer. Am J Transl Res 2021;13:8235-40. [PubMed]
- Chen Z, Liu H, Wang H, et al. Effect of low-frequency rotary magnetic fields on advanced gastric cancer: Survival and palliation of general symptoms. J Cancer Res Ther 2018;14:815-9. [Crossref] [PubMed]
- Lin Y, Docherty SL, Porter LS, et al. Symptom experience and self-management for multiple co-occurring symptoms in patients with gastric cancer: A qualitative study. Eur J Oncol Nurs 2020;49:101860. [Crossref] [PubMed]
- Scarpi E, Dall'Agata M, Zagonel V, et al. Systematic vs. on-demand early palliative care in gastric cancer patients: a randomized clinical trial assessing patient and healthcare service outcomes. Support Care Cancer 2019;27:2425-34. [Crossref] [PubMed]



