
Rare cases of atraumatic splenic rupture managed conservatively in patients with myeloid neoplasms: a report of two cases and literature review
Highlight box
Key findings
• Two case reports of atraumatic splenic rupture (ASR) associated with myeloid neoplasms are presented. One patient with chronic myelomonocytic leukemia developed ASR after 5-azacytidine treatment, and the other in the blast phase of myeloproliferative neoplasms experienced ASR during disease progression.
What is known and what is new?
• ASR is rare, mainly caused by underlying pathological conditions like neoplastic diseases, and surgery has been the traditional treatment.
• Reports on conservative management of ASR related to myeloid neoplasms are scarce. Our cases show potential for conservative management in such patients.
What is the implication, and what should change now?
• Patients may achieve acceptable outcomes with conservative management. More research is required to establish clear guidelines for conservative management of ASR in this patient population.
Introduction
Rupture of the spleen without trauma or pre-diagnosed disease, termed atraumatic splenic rupture (ASR), is a rare yet life-threatening condition. Approximately 7% of ASR cases remain idiopathic, while a significant majority, accounting for 93%, are caused by underlying pathological factors (1). Infection such as infectious mononucleosis, malaria, coronavirus disease 2019 (COVID-19) (2), and dengue-infection (3), neoplastic disease, particularly haematologic (leukemia, lymphoma) and other non-haematologic neoplasms (4), as well as inflammatory diseases (5) are the main causes for this condition. Acute leukemia (1,6) and chronic myelomonocytic leukemia (CMML) (7-9) are frequently reported in cases of ASR associated with hematological myeloid neoplasms. Splenectomy is the standard treatment for splenic rupture (1). Given the increased preoperative and postoperative risks associated with splenectomy, some studies have proposed the use of non-surgical management in managing ASR (10,11). In the report, we present the clinical data and the outcomes of conservative management for ASR associated with myeloid neoplasms, one with CMML and the other with blast phase MPN (MPN-BP). We present this article in accordance with the CARE reporting checklist (available at https://cco.amegroups.com/article/view/10.21037/cco-24-122/rc).
Case presentation
Case 1
In July 2020, a 74-year-old female patient presented to the Department of Hematology, First Teaching Hospital of Tianjin University of Traditional Chinese Medicine, complaining of fatigue, and a history of type 2 diabetes, hypertension, and hyperuricemia. The complete blood counts (CBC) revealed a white blood cell (WBC) count of 11.1×109/L, a monocyte count of 1.28×109/L, a platelet count of 56×109/L, and a hemoglobin level of 91 g/L. The patient was reluctant to undergo bone marrow examination and was treated with red blood cell transfusion.
The patient presented to the Department of Hematology, First Teaching Hospital of Tianjin University of Traditional Chinese Medicine again in January 2022. The CBC revealed a WBC count of 47.8×109/L, absolute monocytosis (12×109/L), a hemoglobin level of 77 g/L, and a platelet count of 40×109/L. Peripheral blood smear revealed 25% monocytes. The bone marrow aspiration showed hypercellularity, dysplastic monocytes with 11% monocytic precursors. Chromosome study results showed 46, XY, r(18)[20] without Philadelphia chromosome. Next-generation sequencing detected a CBL missense mutation and an ASXL1 deletion mutation. The absence of both the BCR::ABL1 fusion gene and driver mutations within Janus kinase 2 (JAK2), myeloproliferative leukemia, or the CALReticulin gene significantly contributed to ruling out the diagnosis of MPN. No splenomegaly was detected by computed tomography (CT) (Figure 1A). The diagnosis of CMML was made according to the 5th edition of the World Health Organization classification of haematolymphoid tumours (12). The patient received initial cytoreductive therapy with hydroxyurea. When WBC dropped, 5-azacitidine was administered subcutaneously at a daily dosage of 100 mg for seven consecutive days. During 5-azacitidine administration, the WBC count gradually escalated, whereas the platelet count gradually decreased. The patient presented with a sudden onset of abdominal pain with diffuse tenderness, starting from the left upper abdomen and subsequently spreading to generalized abdominal pain on the second day following hypomethylating treatment. Her vital signs were as follows: temperature, 36.5 °C; heart rate, 110 beats/min; blood pressure, 73/34 mmHg. Promptly, fluid resuscitation was administered to stabilize the patient’s arterial blood pressure, followed by red blood cell transfusion. In response to the treatment, a gradual increase in arterial blood pressure and a decrease in heart rate were observed. Once her condition had stabilized, approximately 24 hours later, an abdominal ultrasound examination was performed and revealed moderate splenomegaly measuring 13.9 cm, along with a mixed echogenic region of 8.4 cm × 4.3 cm located at the lower pole of the spleen. Future confirmation of splenic parenchymal hemorrhage was provided by abdominal CT imaging (Figure 1B).
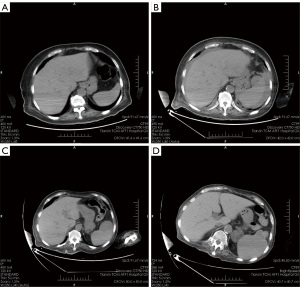
Furthermore, the presence of free intraperitoneal fluid indicated splenic rupture, and splenic contrast-enhanced ultrasound confirmed a focal capsular breach with a visible contrast leakage approximately 3 mm wide. The patient reported no prior history of trauma and denied any other potential causes of increased intra-abdominal pressure, including constipation. Additionally, she did not exhibit symptoms of fever, ruling out splenic infection or inflammation as possible causes. After a thorough evaluation, a diagnosis of ASR was established. Since she responded well to fluids and red blood cell transfusion, splenectomy was deemed unnecessary. Instead, a non-operative management approach was employed, including platelet transfusions and antibiotics. Her hemoglobin level stabilized following the administration of six units of red blood cell on day 4, indicating that the bleeding had ceased. Furthermore, her severe abdominal pain significantly improved after seven days. An ultrasound scan conducted ten days later revealed the resorption of perisplenic effusions. Over several months, there was a notable regression of the intrasplenic hemorrhage, as depicted in Figure 1C, signifying a favorable evolution. Additionally, calcification occurred in the chronic phase, as shown in Figure 1D. Subsequently, she was treated with hydroxyurea for leukocytosis. However, she succumbed to leukemia transformation approximately 18 months later. Due to the patient’s family refusal of an autopsy, a histopathological examination of the spleen could not be conducted. Figure 2 shows the timeline of events.
Case 2
Patient 2 was a 52-year-old woman who had been diagnosed with JAK2V617-postive essential thrombocythemia (ET) eight years ago, confirmed by bone marrow examination. Since then, she had been successfully treated with hydroxyurea. In April 2023, she was referred to the Department of Hematology, First Teaching Hospital of Tianjin University of Traditional Chinese Medicine due to progressive fatigue. Her CBC revealed a WBC count of 1.3×109/L, a hemoglobin level of 59 g/L, and a normal platelet count of 252×109/L. General examination revealed no splenomegaly or hepatomegaly. The bone marrow aspirate exhibited hypocellularity, closely resembling the characteristics of peripheral blood, and contained 0.5% blasts. The biopsy specimens revealed global hypoplasia accompanied with grade 2 reticulin fibrosis. Chromosome study revealed a complex karyotype: 43,XX,der(3;17)(q10;q10);add(5)(q11.1);7;der(12)t(12;13)(p13;q11);-13;der(16)t(3;16)(p21;q24);?der(16)t(3;16)[3]. The JAK2V617 allele burden was measured at 15.11%. Mutation analysis for JAK2 exon12, MPL, and CALR was negative. Taken together, these findings supported the diagnosis post-ET myelofibrosis (MF). Subsequently, hydroxyurea treatment was discontinued, and danazol therapy was initiated to manage the anemia.
In June 2023, the patient presented with severe bone pain. The diagnosis of MPN-BP was confirmed (12), supported by the detection of 24% blasts in the bone marrow. CT scans did not reveal any signs of splenomegaly (Figures 3A). Consequently, the patient was administered a hypomethylating agent, decitabine, at a dose of 20 mg/m2 per day as an intravenous infusion for five consecutive days. The patient expressed discomfort in the sacrococcygeal region. However, a CT scan of the lumbar spine, conducted on the second day following decitabine treatment, did not reveal any apparent signs of infection or tumor in that region. Nevertheless, the scan revealed a notable enlargement of the spleen (Figure 3B), indicative of disease progression. Given her reluctance to pursue intensive chemotherapy, she was discharged on the 14th day after decitabine treatment.
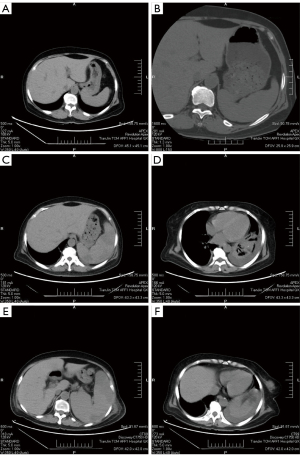
Seven days after experiencing progressive abdominal pain, the patient returned to the hospital on the 20th day following her discharge. During the physical examination, it was observed that the abdominal pain was localized to the left upper quadrant without rebound tenderness. Her temperature upon admission was 38.0 °C, with a heart rate 114 beats/min, a blood pressure of 123/74 mmHg, and a respiration rate of 18 breaths/min. Ultrasound examination revealed significant splenomegaly measuring 19 cm in size, along with multiple hypoechoic regions, the largest of which measured 7.1 cm × 4.0 cm. Abdominal CT scans further confirmed splenic parenchymal hemorrhage (Figure 3C) and perisplenic hemorrhage (Figure 3D). The patient denied any history of abdominal trauma or other conditions that could lead to increased intraperitoneal pressure, such as constipation. Based on these findings, a diagnosis of ASR was made. Given her stable hemodynamics, a conservative approach with close monitoring was adopted. She underwent transfusions of red blood cells, platelets, and antibiotics. Although her hemoglobin level remained stable for the initial four days following the administration of two units of red blood cells, it unexpectedly fluctuated on the fifth day, indicating ongoing splenic bleeding. On day 9, her WBC count escalated to 28×109/L, while ultrasound revealed a spleen size measuring 22.3 cm. CT scans consistently demonstrated persistent perisplenic and parenchymal hemorrhage (Figure 3E,3F). Given her deteriorating performance status, it was deemed inappropriate to administer systemic chemotherapy. Seventeen days after the diagnosis of ASR, she succumbed to a pulmonary infection. As the patient’s family had not consented to an autopsy, histopathological examination of the spleen could not be conducted. Figure 4 shows the timeline of events.

All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committees and with the Helsinki Declaration and its subsequent amendments. Written informed consent was obtained from the patients for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
The onset of ASR can be insidious, presenting significant diagnostic challenges and posing a life-threatening risk due to potential delays in diagnosis and treatment. The clinical presentations observed in our two cases emphasize the critical importance of evaluating the spleen using ultrasound or CT scans in patients with myeloid neoplasms experiencing left upper abdominal pain associated with decreasing hemoglobin levels. Importantly, even in the absence of splenomegaly, the possibility of ASR should be considered, as it may result from rapid splenic expansion.
Splenectomy has long been regarded as the standard treatment for splenic rupture (1). A particular study incorporated 17 dengue-infected patients with ASR (3). Among them, 12 patients (70.6%) underwent immediate splenectomy, while the remaining 5 received conservative treatment. However, two of those on conservative treatment had painful recurrence, which ultimately necessitated delayed splenectomy. What is more concerning is the high mortality rate. Among the 17 patients, 4 patients died, with an overall mortality rate of 23.5%. Three of these deaths occurred after splenectomy, caused by sepsis, multiorgan failure, and coagulopathy despite numerous blood transfusions. These cases highlight the high mortality and risks associated with splenectomy in dengue-infected ASR patients (3). Studies have suggested that non-surgical management, encompassing splenic artery embolization and conservative medical treatment, represents a viable treatment alternative for ASR (10,11). This is particularly applicable to patients with hematological malignancies. Given their overall health status and the presence of severe thrombocytopenia, surgical exploration is deemed to carry significant risks. The selection of the treatment plan mainly depends on the severity of ASR and the patient’s hemodynamic stability. By carefully evaluating these factors, medical professionals can make a more well-informed and suitable treatment decision for patients. In our study, both patients underwent conservative therapy, yet their outcomes differed. In the case of the first patient, despite experiencing hemodynamic instability, she responded favorably to fluid resuscitation and blood transfusion within 24 hours. Her condition improved significantly, with resolution of shock and stabilization of hemoglobin levels. Furthermore, a remarkable reduction in perisplenic effusions was observed on CT scans ten days later. This experience taught us that a prompt diagnosis coupled with a conservative approach was effective in managing the patient with CMML, ultimately eliminating the need for splenectomy.
On the other hand, the second patient initially exhibited hemodynamic stability upon the occurrence of ASR, yet her prognosis was grim due to progressive splenomegaly, subsequent uncontrolled leukocytosis, and recurrent parenchymal hemorrhage. Therefore, through the treatment experience of this patient, we can recognize that aggressive therapeutic strategies, including spleen embolization or splenectomy, might be warranted for patients with ASR associated with MPN-BP, similar to the approach taken for AML patients who undergo ASR (6,11).
The precise mechanism underlying ASR remains unknown, but it appears to be associated with pathological spleens rather than normal ones. Most ruptured spleens display moderate to severe enlargement (13), indicating that splenic enlargement itself poses a great risk for ASR. Some myeloid neoplasms, particularly MPN (14), although commonly characterized by splenic involvement and increased spleen volumes, infrequently exhibit associations with ASR. It is hypothesized that, apart from the degree of splenic enlargement, the rapidity of its expansion contributes to the variable occurrences of ASR. Rapid splenic expansion, coupled with inadequate blood supply, can lead to infarction, rendering the spleen susceptible to fragility. Both acute leukemia and MPN patients exhibit splenomegaly, yet their histopathological manifestations differ significantly. In acute leukemia, the infiltration of blats cells primarily leads to the destruction of the splenic structure (6). On the other hand, while MPN patients also display blasts in the spleen (15), the primary pathological changes are extramedullary hematopoiesis (15) and angiogenesis (16). Coagulation disturbances resulting from hyperleukocytosis or thrombocytopenia can also contribute to splenic hemorrhage in acute leukemia (17).
Conclusions
Here, we report two cases of ASR in myeloid neoplasms, demonstrating that patients may achieve acceptable outcomes with conservative management.
Acknowledgments
None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://cco.amegroups.com/article/view/10.21037/cco-24-122/rc
Peer Review File: Available at https://cco.amegroups.com/article/view/10.21037/cco-24-122/prf
Funding: The study was supported by
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://cco.amegroups.com/article/view/10.21037/cco-24-122/coif). All authors report the funding from the National Natural Science Foundation of China (No. 82104785). The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committees and with the Helsinki Declaration and its subsequent amendments. Written informed consent was obtained from the patients for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Renzulli P, Hostettler A, Schoepfer AM, et al. Systematic review of atraumatic splenic rupture. Br J Surg 2009;96:1114-21. [Crossref] [PubMed]
- Lucido FS, Nesta G, Gambardella C, et al. Atraumatic splenic rupture in COVID-19 era: case report and systematic literature review. Minerva Surg 2023;78:86-91. [Crossref] [PubMed]
- Radwan I, Magdy Khattab M, Mahmoud AR, et al. Systematic review of spontaneous splenic rupture in dengue-infected patients. Rev Med Virol 2019;29:e2029. [Crossref] [PubMed]
- Aubrey-Bassler FK, Sowers N. 613 cases of splenic rupture without risk factors or previously diagnosed disease: a systematic review. BMC Emerg Med 2012;12:11. [Crossref] [PubMed]
- Nadaraja R, Yahya Z, Mori K, et al. Atraumatic splenic rupture in patient with acute pancreatitis. BMJ Case Rep 2021;14:e238559. [Crossref] [PubMed]
- Hajri A, Yaqine K, El Massi S, et al. Spontaneous splenic rupture: A rare complication of acute myeloid leukemia. Report of a case. Ann Med Surg (Lond) 2021;65:102286. [Crossref] [PubMed]
- Pophali P, Horna P, Lasho TL, et al. Splenectomy in patients with chronic myelomonocytic leukemia: Indications, histopathological findings and clinical outcomes in a single institutional series of thirty-nine patients. Am J Hematol 2018;93:1347-57. [Crossref] [PubMed]
- Nie Y, Kent A, Do M, et al. Atraumatic Splenic Rupture due to Chronic Myelomonocytic Leukemia Treated with Partial Splenic Artery Embolization. Case Rep Oncol 2022;15:277-84. [Crossref] [PubMed]
- Abbasi AM, Adil S, Moiz B. Spontaneous splenic rupture - An uncommon complication of chronic myelomonocytic leukemia. Leuk Res Rep 2020;14:100205. [Crossref] [PubMed]
- Mokashi AJ, Shirahatti RG, Prabhu SK, et al. Pathological rupture of malarial spleen. J Postgrad Med 1992;38:141-2. [PubMed]
- Gnanapandithan K. Atraumatic splenic rupture in acute myeloid leukemia. Cleve Clin J Med 2019;86:715-6. [Crossref] [PubMed]
- Khoury JD, Solary E, Abla O, et al. The 5th edition of the World Health Organization Classification of Haematolymphoid Tumours: Myeloid and Histiocytic/Dendritic Neoplasms. Leukemia 2022;36:1703-19.
- Barrier JH, Bani-Sadr F, Gaillard F, et al. Spontaneous rupture of the spleen revealing primary human immunodeficiency virus infection. Clin Infect Dis 1997;25:336-7. [Crossref] [PubMed]
- Baba M, Tanahashi N, Seno K, Nara M, Shinbo T. Myelofibrosis with marked subcapsular bleeding of the spleen--a case report. Rinsho Ketsueki 1990;31:669-73. [PubMed]
- Wang X, Prakash S, Lu M, et al. Spleens of myelofibrosis patients contain malignant hematopoietic stem cells. J Clin Invest 2012;122:3888-99. [Crossref] [PubMed]
- Barosi G, Rosti V, Massa M, et al. Spleen neoangiogenesis in patients with myelofibrosis with myeloid metaplasia. Br J Haematol 2004;124:618-25. [Crossref] [PubMed]
- Biswas S, Keddington J, McClanathan J. Large B-cell lymphoma presenting as acute abdominal pain and spontaneous splenic rupture; a case report and review of relevant literature. World J Emerg Surg 2006;1:35. [Crossref] [PubMed]



