
The histological prevalence and clinical implications of folliculotropism and syringotropism in mycosis fungoides
Introduction
Cutaneous T-cell lymphomas are a heterogeneous group of extranodal non-Hodgkin lymphomas of which approximately 50% are comprised of mycosis fungoides (MF). Per the WHO-EORTC classification of cutaneous lymphomas, conventional MF may be differentiated from three distinct subtypes: solitary pagetoid reticulosis, folliculotropic MF, and granulomatous slack skin (1). Evidence in the literature further promotes syringotropic MF as an additional clinicopathological variant (2).
Clinical conventional MF may present in a myriad of forms, typically patches, plaques, or tumorous nodules with the chief histopathologic criteria being epidermotropism (3). The variants of MF have their own distinctive clinical presentations; syringotropic MF, for instance, typically presents on the palms and soles (4) and folliculotropic MF typifies a more aggressive, acneiform presentation (5). Apart from epidermotropism, on histopathology, syringotropic MF features a syringotropic lymphocytic infiltrate occasionally surrounding hyperplastic eccrine glands and eccrine ducts (4), while folliculotropic MF is noted by folliculotropism, the presence of neoplastic T-lymphocytes infiltrating the hair follicle epithelium, sometimes sparing the epidermis (6,7).
As of now, incidence of MF is approximately 0.36 per 100,000 (8) but we found no reported incidence of the subtypes of MF on literature review to date, with the exception of one study, noting fewer than 50 documented cases of syringotropic MF (4,9). While the majority of studies referencing folliculotropic and syringotropic MF particularly label these findings as rare in the scope of clinical MF, folliculotropism and syringotropism in the context of MF may not be nearly as uncommon. For reasons unknown, patients with clinically conventional MF may present with folliculotropism or syringotropism on histopathology but not necessarily be diagnosed with clinical folliculotropic or syringotropic MF. Per literature review, there is a clear disconnect between the clinical presentation of folliculotropic MF and syringotropic MF and the histopathological diagnosis of folliculotropism and syringotropism. In one study, folliculotropism and syringotropism were more prominent than epidermotropism in 36% and 40% of cases of conventional MF, respectively (10).
Moreover, minimal research has been done exploring what these histopathological findings mean to staging and clinical outcome. Surprisingly, the presence of folliculotropism and syringotropism are currently not assessed nor documented on histopathology reports and thus largely ignored in clinical practice, within the literature, and in NCCN guidelines. Herein we sought to determine an estimated histopathological prevalence within our patient population and how the histopathological diagnosis can translate to clinical practice. Ultimately, we aim to determine if the presence of these histopathological findings may correlate with disease severity or staging.
Methods
This study was conducted with the approval of the Thomas Jefferson University Institutional Review Board. This is a prospective, observational study conducted at the Cutaneous Lymphoma Clinic in the Department of Dermatology and Cutaneous Biology at Jefferson University Hospital and all authors of this study are affiliated with the Cutaneous Lymphoma Clinic. Any patient determined to have MF was enrolled into the study with the exception of those with incomplete documentation, or any patient treated at the Cutaneous Lymphoma Clinic for less than six months. Patients were also excluded if a biopsy from their initial visit at the clinic was not present, as these were the only samples analyzed for presence or absence of syringotropism and folliculotropism in order to reduce any cofounding variables or effect from previous treatment. Eighty-seven patients with clinically diagnosed and biopsy proven MF were identified over an approximate 6-year time period between the years of 2012 and 2018. The diagnosis of MF was determined by utilizing standard diagnostic criteria: clinical presentation, histopathology, clonal TCR gene rearrangement, flow cytometry and immunopathologic expression. Patients with MF having new or morphologically changing skin lesions are biopsied and skin biopsies are specifically examined for the histopathology of the hair follicles and eccrine glands.
This study utilized modified severity weighted assessment tool (mSWAT) to quantify both the body surface area affected in a patient and the severity of the disease. The mSWAT is an analytical tool that configures estimates of total body surface area with the patient’s palms and fingers as relatively 1% body surface area and stratifying the disease burden by multiplying the presentation of patches, plaques, and tumors by 1, 2, and 4 respectively. Three research fellows over the six-year period quantified the mSWAT scores for each patient. The mSWAT value from the initial patient visit at the Jefferson Cutaneous Lymphoma center was recorded and used for analysis.
Severity of disease was further assessed by the presence of pruritus. A visual analog scale on degree of pruritus experienced is provided to each patient per visit. Patients choose a value on a scale from one to ten indicating their degree of pruritus at the beginning of the office visit (0 indicating a score of no pruritus and 10 being the worst pruritus they have ever experienced). These values are charted and treatment progress is tracked by improvements in reported experience. The degree of pruritus for each patient was recorded at their first patient visit at the office. The pruritus value from the initial patient visit at the Jefferson Cutaneous Lymphoma center was recorded and used for analysis.
Finally, the original patient biopsies from the initial patient visit of all subjects were analyzed for folliculotropism and syringotropism status. The mSWAT values and pruritus values were analyzed according to the following groups: folliculotropism only, syringotropism only, folliculotropism and syringotropism, neither folliculotropism or syringotropism. The non-parametric P value was calculated by the Kruskal-Wallis test for numerical covariates and the Fisher’s exact test was used for categorical covariates in regard to pruritus and mSWAT scores.
Results
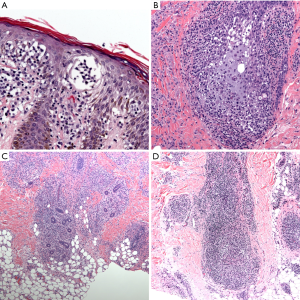
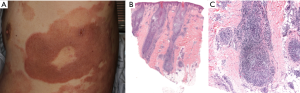
The patient population examined in this study was comprised of 52 men (59.8%) and 35 (40.2%) women with the age range from 22 to 87, mean age of 61.5, and median age 63. Of the 87 patients, 64 were Caucasian (73.6%), 19 were African American (21.8%), 3 Latino (3.4%) and 1 Asian (1.1%). Additionally, of the 87 patients examined, 70 patients (80.5%) exhibited syringotropism in their original biopsy and 68 patients (78.2%) exhibited folliculotropism. Presence of both findings concurrently was in 56 patients (64.4%), while neither finding was present in 5 patients (5.7%). The singular finding of folliculotropism was found in 12 patients (13.8%), while the singular finding of syringotropism was exhibited in 14 patients (16.1%). This information is summarized in Table 1. Examples of the histologic presence of folliculotropism, syringotropism, and both folliculotropism and syringotropism, can be seen in Figure 1.
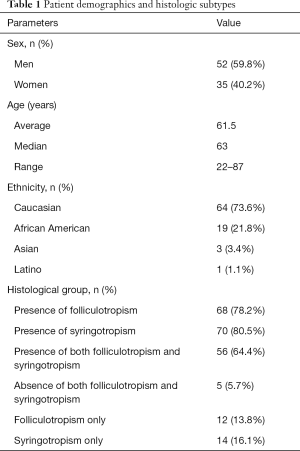
Full table
Number of subjects, and mean, median, minimum values, maximum values and standard deviation of mSWAT scores and reported pruritus in each histological group are summarized in Table 2. Average mSWAT scores for presence of both folliculotropism and syringotropism, folliculotropism only, syringotropism only, and absence of both folliculotropism and syringotropism presentations were 16, 19.9, 19.24 and 39.17 respectively. While there was no statistical significance between the histologic groups in regard to mSWAT (P=0.079, α=0.05), the relative increase in mean and median mSWAT values with the presence of folliculotropism, syringotropism, or concurrent features histologic features, in particular both presentations concurrently, indicate that an increase in patient population could yield statistical significance in the future. Similarly, average reported pruritus values for presence of both folliculotropism and syringotropism, folliculotropism only, syringotropism only, and concurrent folliculotropism and syringotropism presentations were 1, 3.42, 2.89, and 4.2 respectively (P=0.088, α=0.05).
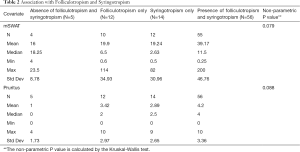
Full table
The association of folliculotropism with pruritus and mSWAT scores is summarized in Table 3. The average, median, minimum, maximum and standard deviation values for mSWAT scores and pruritus values for two histologic groups (presence of folliculotropism and absence of folliculotropism) are reported. The mean mSWAT values for the folliculotropic group and non-folliculotropic group 36.21 and 18.43 respectively (P=0.082, α=−0.05). The non-parametric P value determined by analysis of all values was (P=0.082, α=0.05). The mean pruritus values recorded for presence of folliculotropism and those with an absence of folliculotropism were 4.06 and 2.39 respectively. Analysis of average, median, minimum, maximum and standard deviation values for association of folliculotropism with pruritus values deemed a significant value of 0.043 (α=0.05).
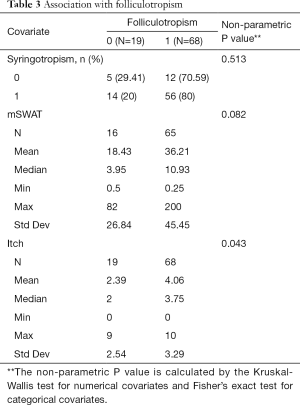
Full table
The association of syringotropism with pruritus and mSWAT scores is summarized in Table 4. The average, median, minimum, maximum and standard deviation values for mSWAT scores and pruritus values for two histologic groups (presence of syringotropism and absence of syringotropism) are reported. The mean mSWAT values for the syringotropic group and non-syringotropic group 35.6 and 18.79 respectively. The non-parametric P value determined by analysis of all values was 0.342 (α=0.05) and therefore pruritus value association for those with a histologic presentation of folliculotropism versus those without was not statistically significant. The mean pruritus values recorded for presence of syringotropism and those with an absence of syringotropism were 3.94 and 2.71 respectively. Analysis of average, median, minimum, maximum and standard deviation values for association of syringotropism with pruritus values was not significant with a P value of 0.156 (α=0.05).
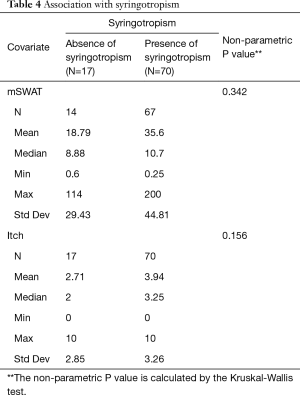
Full table
Discussion
Within our patient population, the male to female ratio is approximately 1.5:1, which mirrors the documented predilection for MF in men. The median age of the patient population is also fairly similar to the median age of 55 recognized within the literature (6).
Despite assertions in the literature stating the paucity of syringotropic and folliculotropic MF, analysis of subject skin biopsies revealed 80% of patients displayed syringotropism, 78% folliculotropism, and 64% concurrent syringotropism and folliculotropism (Table 1). This is likely attributed to our clinical practice of reviewing every MF skin biopsy for the presence of folliculotropism and syringotropism, specifically evaluating the hair follicles and eccrine glands regardless of suspicion for these findings on clinical presentation. Due to the myriad of clinical and histopathological presentations possible in MF, it is likely that these histopathological findings have simply been overlooked in the past.
This observation lends credence to the possibility that folliculotropism and syringotropism may be more prevalent findings central to the MF histopathological spectrum as a whole rather than rare findings isolated to distinct clinical variants. The disconnect between the histopathology and clinical presentation raises the question of if or when the transition from the histopathologic finding to clinical presentation actualizes itself. Ultimately, future research necessitates following the patients examined in this study, noting how many patients with these histopathological findings go on to develop changes in the course of their disease. The potential value of such tracking is immeasurable as physicians may be able to provide a more accurate prognostic assessment of disease progression and can enable future patients to be treated promptly and aggressively in the interest of improving quality of life.
Earlier studies within the literature noted an association of syringotropism with folliculotropism, with one study reporting evidence of eccrine gland involvement in the setting of folliculotropic MF to be 4–33% (9). However in our analysis, of the 68 patients who presented with folliculotropism, 82% presented with concurrent syringotropism. Additionally, only 13.8% of our patient population presented with pure folliculotropism as the sole finding (sans syringotropism) and 16.1% presented with pure syringotropism (sans folliculotropism), while 64% of the patient population presented with both findings (Table 1). These values fall in line with a recent study on a large series of patients with folliculotropic MF, where involvement of the eccrine glands was reported in 56% of cases (11). Our findings suggest that this relationship may be due to an unknown extrinsic confounding factor. A commonality exists between the hair follicle and the eccrine gland that for an unknown reason makes them both susceptible to neoplastic T-cell honing, suggesting that patients with a form of MF affecting a deeper compartment of skin are simply more likely to have multiple deep compartments affected (Figure 2).
While folliculotropic MF is recognized as being a more aggressive variant (5,12), it continues to be unclear as to whether folliculotropism or syringotropism, as distinctive histopathologic variants, have a predilection for greater disease severity with worsening of symptoms, as folliculotropic MF may signify a more aggressive disease course because they are more likely to have lymphocytic infiltration in deeper compartments of the skin. Nonetheless, the association determined here merits further exploration and a possible modification to the current staging algorithm. Per NCCN 2018 guidelines, the diagnosis of folliculotropic MF automatically upstages a patient. In order to provide a more accurate assessment of disease severity, patients with folliculotropism or syringotropism on histopathology may also warrant a higher evaluation of stage.
The importance in expanding the scope of the histopathologic report on suspected MF cases to include syringotropism and folliculotropism lays in the impact it imparts on clinical outcomes. Patients with these histopathological findings had greater percentages of their skin affected by disease or more severe morphology (tumor and plaque), as evidenced by their higher mSWAT scores (Tables 2-4). The mSWAT scores of patients with concurrent folliculotropism and syringotropism were on average 2.45 times higher than patients without either histologic presentation. While not statistically significant due to a smaller patient population inhibiting power, a clinically similar assessment is evidenced when looking at average reported pruritus values for patients with a concurrent histologic presentation compared to those without, with a mean pruritus value 4.2 times higher. When summarizing the data found in our study, it is evident that a trend exists when examining the correlation between these distinct histologic variants and severity of disease as it relates to mSWAT scores and pruritus. Analysis of data demonstrates an increase in average mSWAT scores and pruritus in both syringotropism and folliculotropism presence, and an even greater increase when both variants are found together.
Recognizing pruritus as one of the more tangible assessments of active disease, patients with syringotropism or folliculotropism were also clinically found to report the presence of debilitating pruritus more often than patients without these findings. Furthermore, statistical significance was found between patients exhibiting folliculotropism and pruritus scores, indicating folliculotropism as a prognostic indicator for the symptomatology a patient might experience after diagnosis as it relates to pruritus.
It is apparent that the majority of clinically diagnosed folliculotropic MF and syringotropic MF have more severe degrees of folliculotropism and syringotropism on histopathology, yet from the active analysis of skin biopsies of conventional MF we conclude that folliculotropism and syringotropism are more prevalent than previously recognized. Our study demonstrated a trend that exists between these histologic variants and severity of disease in regard to mSWAT and pruritus. Limitations of our study include the small population number, a difficult factor to modify due to the rarity of MF, and our status as a tertiary referral center which may introduce referral bias as we are more likely to have patients with more difficult disease referred to our center. Our study reveals an obvious trend that lays credence to the fact that the presence of folliculotropism and/or syringotropism correlate with a more severe clinical picture, and therefore an increase in sample size will likely reveal statistically significant results in the future.
Patients diagnosed with MF can be offered more effective treatment if awareness is raised histopathologically. We suggest that histopathology reports formally expand their scope to include the search for, and reporting of, these findings on skin lesions suspicious for MF. Physicians assessing for MF are also recommended to biopsy new skin lesions, lesions recalcitrant to treatment, lesions with changing clinical appearance and to section biopsies until hair follicles and eccrine glands can be evaluated. It is our goal to continue following the disease progression in our patient population to further determine how their histopathological diagnosis translates into clinical presentation and how the prognosis differs from those with conventional MF. Further research is necessary to truly determine the intricate relationship between folliculotropism and syringotropism and how the treatment algorithm for MF can be further refined for patients with these findings.
Acknowledgements
We thank Mitch Finkelstein for his contribution in data collection, helping bring about the completion of this paper.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was conducted with the approval of the Thomas Jefferson University Institutional Review Board.
References
- Willemze R, Jaffe ES, Burg G, et al. WHO-EORTC classification for cutaneous lymphomas. Blood 2005;105:3768-85. [Crossref] [PubMed]
- Thein M, Ravat F, Orchard G, et al. Syringotropic cutaneous T-cell lymphoma: an immunophenotypic and genotypic study of five cases. Br J Dermatol 2004;151:216-26. [Crossref] [PubMed]
- Nashan D, Faulhaber D, Ständer S, et al. Mycosis fungoides: a dermatological masquerader. Br J Dermatol 2007;156:1-10. [Crossref] [PubMed]
- de Masson A, Battistella M, Vignon-Pennamen MD, et al. Syringotropic mycosis fungoides: clinical and histologic features, response to treatment, and outcome in 19 patients. J Am Acad Dermatol 2014;71:926-34. [Crossref] [PubMed]
- Kazakov DV, Burg G, Kempf W. Clinicopathological spectrum of mycosis fungoides. J Eur Acad Dermatol Venereol 2004;18:397-415. [Crossref] [PubMed]
- Demirkesen C, Esirgen G, Engin B, et al. The clinical features and histopathologic patterns of folliculotropic mycosis fungoides in a series of 38 cases. J Cutan Pathol 2015;42:22-31. [Crossref] [PubMed]
- Wang L, Wang G, Gao T. Granulomatous syringotropic mycosis fungoides with two lesions having reactive B-cell proliferation. J Cutan Pathol 2014;41:400-6. [Crossref] [PubMed]
- Weinstock MA, Gardstein B. Twenty-year trends in the reported incidence of mycosis fungoides and associated mortality. Am J Public Health 1999;89:1240-4. [Crossref] [PubMed]
- Bakar Ö, Seçkin D, Demirkesen C, et al. Two clinically unusual cases of folliculotropic mycosis fungoides: One with and the other without syringotropism. Ann Dermatol 2014;26:385-91. [Crossref] [PubMed]
- Rongioletti F, Smoller B. The histologic value of adnexal (eccrine gland and follicle) infiltration in mycosis fungoides. J Cutan Pathol 2000;27:406-9. [Crossref] [PubMed]
- Pileri A, Facchetti F, Rütten A, et al. Syringotropic mycosis fungoides: a rare variant of the disease with peculiar clinicopathologic features. Am J Surg Pathol 2011;35:100-9. [Crossref] [PubMed]
- Lehman JS, Cook-Norris RH, Weed BR, et al. Folliculotropic mycosis fungoides: single-center study and systematic review. Arch Dermatol 2010;146:607-13. [Crossref] [PubMed]


