Hepatocellular carcinoma in the modern era: transplantation, ablation, open surgery or minimally invasive surgery?—A multidisciplinary personalized decision
Introduction-general concepts
The earlier diagnosis, coupled with advances in operative and postoperative management and patient selection have increased survival after hepatectomy for hepatocellular carcinoma (HCC) (1). Survival rates from HCC in the United States have doubled over the past 2 decades (2).
The two most frequently used curative treatments for HCC are surgical resection and orthotopic liver transplantation (OLT) transplantation. In patients with advanced cirrhosis and tumors within transplantation criteria, in the absence of extrahepatic spread and macrovascular invasion, liver transplantation is the gold standard, as it allows treatment of the tumor and the underlying cirrhosis as well. In patients with well-preserved hepatic function (Child-Pugh grade A and early Child-Pugh grade B) and resectable disease, surgical resection is the most appropriate treatment (3-6).
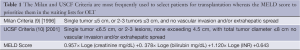
For years, selection of candidates for resection has been based on the Child-Pugh classification, however even Child-Pugh A patients may already have liver functional impairment with clinically significant portal hypertension (7). A normal serum bilirubin level and the absence of clinically significant portal hypertension (i.e., hepatic vein pressure gradient <10 mmHg) appear to predict a low risk of postoperative liver failure after hepatectomy (8). Other researchers have emphasized that the Model of End-Stage Liver Disease (MELD) score (Table 1) can be a useful predictor of postoperative liver failure (11). In Japan, the indocyanine green retention rate is used to identify the best candidates for resection. The hepatocyte clearance of indocyanine green (ICG), an anionic dye, in the bile at 15 minutes is used to evaluate the hepatocyte function (12). A value of 40% retention suggests severe liver dysfunction and prohibits surgical resection (13).
Full table
The care of HCC patients was revolutionized after a landmark publication, that established OLT as therapy for HCC patients with cirrhosis, by Mazzaferro et al. (9) in 1996. It showed that patients with up to 3 foci of HCC each less than 3 cm in size or one tumor measuring less than 5 cm, without vascular invasion or extrahepatic spread (known as the “Milan criteria”) experienced a 5-year overall survival rate that was comparable to the survival rates of cirrhotics undergoing transplant without cancer (75%) with recurrence-free survival rate of 83%. Before that, it was known that transplantation was associated with a significant disease free survival for 3 or fewer tumors each within 3 cm compared to resection (14).
The Milan criteria have been validated (10,15,16) and are used for selection of patients in the USA and Europe, and accepted by the United Network for Organ Sharing (UNOS).
Subsequently, researchers in the University of California at San Francisco (UCSF), broadened the criteria to include single tumors measuring less than 6.5 cm or 2-3 tumors, none greater than 4.5 cm in size, with total tumor diameter not greater than 8 cm (Table 1) (10). The initial study revealed no adverse impact on survival (5-year overall survival rate 75%). However it was criticized as the tumor characteristics were obtained at the time of explantation. Subsequently, prospective validation of the UCSF criteria based on preoperative imaging yielded similar results (17). Patients meeting UCSF criteria had similar 5-year survival as patients meeting Milan criteria both by preoperative imaging (18,19).
The MELD score (Table 1), was implemented in 2002 in an effort to quantify liver insufficiency and prioritize patients in waiting lists for OLT according to their mortality risk. Additional points were allotted to patients with HCC to equilibrate their mortality risk in relation to the mortality of end-stage cirrhosis. Patients with at least a solitary lesion that is greater than 2 cm in size are awarded 22 MELD points (20-22), adjusted every 3 months to reflect a 10% increase in mortality.
The UNOS criteria specify that patients eligible for liver transplantation should not be resection candidates. Only candidates with Stage II HCC are upgraded on the waiting list to a MELD score of 22 (equivalent to a 15% probability of candidate death within 3 months) with the intent to shorten their waiting time. An additional point every 3 months is granted based on the 20-50% dropout rate seen at 1 year due to progression of disease (15). One should always be aware that wait times can vary considerably among regions (23).
Patient eligibility is further being broadened with the use of neo-adjuvant liver-directed therapies. A favorable response to liver-directed therapies prior to transplant resulting in tumor down-staging to within Milan or UCSF criteria coupled with a surveillance period to select individuals that will remain transplantable allows patients with higher stage tumors to receive a transplant and experience similar cancer-specific survival.
In this context, we will examine the controversial areas between surgical resection, transplantation and ablation and give an overview of the recent advances in minimally invasive surgery.
Early hepatocellular carcinoma: surgical resection versus ablation
Ablative techniques destroy tumor via temperature changes [radiofrequency (RFA), microwave (MWA), cryotherapy or lase] while causing minimal damage to adjacent, normal liver, by injection of chemicals (ethanol, acetic acid) or by combination of the above. The combination of HCC of a soft tumor surrounded by a fibrotic liver makes HCC an ideal target for ablation (24).
The most commonly used ablation techniques are RFA and MWA with radiofrequency ablation being usually the first line (25). Although most ablations are done percutaneously, open surgery offers some advantages as percutaneous approaches cannot assess the abdomen for extrahepatic disease or additional hepatic disease detectable with intraoperative US (26).
In a review that included 95 studies between 1990-2004 and 5,224 ablated tumors, 2,369 of which being hepatocellular cancer, surgical ablation (open or laparoscopic) was superior to percutaneous. Local recurrences were 14% for tumors ≤3 cm and increased to 25% for tumors 3-5 cm and to 58% for tumors >5 cm (27). In a prospective cohort of 218 patients who underwent RFA for lesions ≤2 cm and were followed for a median of 31 months, overall 5-year survival was 55% and it was 68.5% for 100 patients who were considered potential candidates for resection. However, the overall 5-year risk of recurrence was as high as 80% (28).
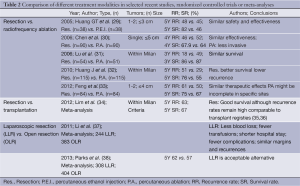
Randomized controlled trials have compared the recurrence and survival rates of ablation vs. resection with variable results which are summarized in Table 2 (29-33).
Full table
Huang et al. (29) randomized 76 patients with 1 or 2 tumors ≤3 cm to surgical resection and percutaneous ethanol injection and found no statistically different 5-year disease free rates (45% vs. 48%, respectively) and survival rates (46% vs. 82%, respectively) concluding equal effectiveness. Chen et al. (30) randomized 161 tumors ≤5 cm to percutaneous ablation or surgical resection and reported similar 4-year disease free rates (46% vs. 52%, respectively) and survival rates (67.9% vs. 64%, respectively). Huang et al. (32) randomized 230 patients within Milan criteria to percutaneous ablation for 115 and surgical resection for another 115 and found 5-year disease free rates (29% vs. 51%, respectively) and survival rates (55% vs. 76%, respectively) concluding that surgical resection was associated with better survival and lower recurrence. A smaller trial of 105 patients with tumors within Milan criteria, randomized them to surgical resection for 54 and percutaneous ablation with RFA or MWA for 51 and reported 3-year disease-free survival were 82% vs. 51% and 86% vs. 87% respectively which were not statistically significant and concluded similar results (31). A more recent trial of 1-2 tumors of ≤4 cm comparing resection (n=84) and RFA (n=84) found 3-year survival rates of 75% and 67% respectively and recurrence-free survival rates 61% and 50%, respectively, concluding similar therapeutic effects but percutaneous RFA more likely to be incomplete at specific sites (33).
However, these trials have been met with some skepticism as they have power limitations, treatment allocation and consent withdrawal issues whereas patients were not always followed in an intention-to-treat manner. Further evidence is needed before drawing definite conclusions.
A recent meta-analysis of small HCC treated with RFA (n=441) or resection (n=436) found higher 5-year recurrence free and survival rates for the resection group whereas in a subgroup analysis of tumors ≤3 cm resection offered improved 3-year survival rates (39).
Another meta-analysis and cost-effectiveness with Markov modeling found that RFA has a similar life expectancy and lower cost for single tumors <2 cm, resection had better life expectancy and cost-effectiveness for single tumors 3-5 cm whereas for 2-3 tumors ≤3 cm similar life expectancy and better cost-effectiveness for RFA (40).
Other studies focusing on long term outcomes for tumors <3 cm found a superiority of resection compared to ablation (41,42) whereas long term results for single tumors <7 cm comparing resection to embolization/ablation suggest that their might be a place for a combination of embolization and ablation of larger tumors (43).
Although the heterogeneity of findings necessitates more prospective randomized studies, especially from Western groups, before making definite conclusions many groups consider RFA as an effective alternative to resection for small (≤3 cm) HCC. The success of ablation decreases significantly in tumors measuring larger than 3 cm (44) and is not recommended for tumors larger than 5 cm (45).
Localized hepatocellular carcinoma: resection versus transplantation
Not every HCC patient is eligible for both resection and transplantation. Many of the HCC patients who undergo curative surgery harbor tumors beyond any criteria of transplantation. For example, resection is the only curative option for patients with large tumors and preserved liver function. The OS rate for patients with tumors greater than 10 cm is still approximately 40%, which is comparable oftentimes with survival in patients with smaller tumors (46). At the same time for many transplanted patients the degree of compromise of their liver function does not allow a safe resection. OLT is clearly the choice for patients with significant cirrhosis, although advanced cirrhosis is associated with a worse outcome even after OLT (35). Outcomes of liver resection are poorer for multifocal HCC and some authors argue against resection for multifocal tumors although it can offer good survival rates in some patients. Liver transplantation addresses HCC along with its multifocal potential and underlying cirrhosis.
One of the controversial areas is the choice between surgery and transplantation for cirrhotics with local, early stage lesions and good hepatic reserve (Child-Pugh A). The UNOS transplantation criteria oversimplify this dilemma by stating that resection candidates are excluded from eligibility for transplantation. When HCC is endemic and the number of affected patients is large, guidelines are leaning towards recommending surgical resection as a first-line treatment option for patients with early HCC who have good liver function (47,48). The main benefits of surgery for this patient population are the comparable survival, the avoidance of long waiting periods for an OLT with danger of disease progression as well as the avoidance of lifelong immunosuppression. Patients within Milan criteria appear to have similar survival after resection or transplantation (49). The benefits of transplantation are the lower recurrence rates in stage-matched patients compared to resection (50). The higher recurrence rates associated with resection vs. OLT, have made some authors suggesting OLT for tumors within Milan criteria who have good liver function (34,51). True recurrence usually arises within the first 2 years after resection and are related to tumor characteristics such as microvascular invasion, satellites and multifocal disease, whereas late recurrences are related to de novo tumors due to the underlying cirrhosis (52-55). However, a recent review of tumors within Milan criteria who underwent curative intent surgical resection concluded that although recurrence rates are high the median overall survival at 5-year was 67% and is improving the recent years (34). When examining results from liver transplant registries such as the Organ Procurement and Transplantation Network and the European Liver Transplant Registry, involving 4,482 and 8,273 patients respectively, the 5-year survival rates of 51% and 60% respectively (35,36) in contrast to the rates of 70 per cent cited by high-volume established centers(9,56).
Salvage transplantation, is a technique which allows some patients to be treated effectively with resection, and offers OLT to patients whose cancer would recur after resection (57-59). Most of the recurrences after resection occur in the liver and the majority of those are still eligible for a transplantation (49). Some researchers believe that the outcomes after salvage transplantation are similar to using transplantation as the first therapeutic choice i.e., without resection (60,61). This is supported by a recent meta-analysis as well (62). Others have expressed concern that operative mortality and recurrence rates are higher (63). The histopathologic information obtained at resection can also be used as a means to immediate listing for salvage transplantation or not. These represent interesting therapeutic strategies and more data are needed (57).
Another controversial area is the use of neoadjuvant more accurately called converison treatment to higher stage tumors and subsequent transplantation. The Barcelona Clinic Liver Cancer Group has demonstrated 5-year survival ≥50% using expanded criteria, or downstaging to Milan criteria with neoadjuvant therapies (64,65). Recently neoadjuvant TACE was successfully used to downstage 24% stage III/IV tumors to within Milan criteria and, subsequently OLT resulting in 94% survival after limited follow-up of 20 months (66). Yao et al. (67) reported that in carefully selected patients effective downstaging can be achieved in the majority followed by an observation period of 3 months minimum, and for the 57% of their patients who received an OLT the 4-year post-transplant survival was 92%. The strategy of adjuvant treatments while waiting for transplantation appears to be cost-effective for patients with anticipated waiting times longer than 1 year (68). Physicians are recommended to treat patients whose wait-list time exceeds 6 months (69,70).
Donor availability is a crucial factor in the decision making as tumors can progress during the waiting period and impede transplantation (71). Anywhere from 18% up to 50% of patients can progress beyond the Milan criteria while waiting for a transplant (15,35,72). In a study by Yao and colleagues, a 6-month waiting period for LT was associated with a 7.2% cumulative dropout probability, increasing to 55.1% at 18 months (73). Policies for transplantation aim to prioritize the sickest patients (74). Intention-to-treat analysis shows that waiting times for liver donors result in decreasing the 2-year survival from 84% to 54% and result in 5-year overall survival rates of 50-60% due to tumor progression (15). Geographic differences in waiting periods can significantly affect the decision to choose transplantation or not for early stage disease (23).
Efforts to address the large waiting list of LT candidates and to decrease the dropout rate have included new transplantation strategies (living donor, domino, split, use of extended criteria donors, and donors after cardiac death). Liver donor grafts offer shorter waiting times however there are concerns that are associated with much higher recurrence rates compared to patients who receive a cadaveric transplant after being in an observation period for a time period appropriately selective those with a less aggressive tumor biology (75). A recent meta-analysis found decreased disease free survival associated with living donor liver transplantation compared to deceased donor liver transplantation (76). However, most available data are retrospective and heterogeneous; prospective studies are needed in order to delineate under which circumstances different transplant methods should be used.
Minimally invasive surgery for hepatocellular carcinoma
Laparoscopic and robotic surgeries are being increasingly used for hepatic resections. Although the amount of existing data is limited, there is growing evidence that laparoscopic surgery is associated with lower perioperative morbidity and postoperative ascites in patients with cirrhosis and appears to have similar oncologic outcome with adequate surgical margins and long-term survival (77).
The smaller, non-anatomic resections preserve liver parenchyma which might be crucial for patients with marginal hepatic function. Advantages which are met in laparoscopic surgery in general, such as less analgesia, smaller incisions, better cosmetic result, and faster discharges are applicable for HCC patients as well. A recent meta-analysis of the existing experience showed less blood loss, fewer transfusions, shorter hospital stay and fewer complications with no differences in surgical margins and tumor recurrences (37). On the other hand, inability to tolerate pneumoperitoneum and extensive adhesions preclude the use of laparoscopic liver resection (LLR), it entails a learning curve, major bleeding might be difficult to control laparoscopically and there are procedure-specific risks such as gas embolism (78).
There are no prospective randomized clinical data comparing laparoscopic or robotic surgery to open surgery. In a large retrospective study, 116 patients underwent laparoscopic liver resection for HCC reporting a 5-year survival rate of approximately 60% (79). In a matched pair study of 42 LLR with equal open resections laparoscopic surgery appeared oncologic adequate with no differences in surgical margins and disease recurrence at 30 months (80). Adequate surgical margins are important as a RCT comparing wide (2 cm) to narrow (1 cm) resection margins in solitary HCC patients reported decreased disease recurrence and improved survival for the wide margin group (81). A recent review of the international experience with laparoscopic liver resection found 5-year survival rates comparable to open hepatic resections (78). A meta-analysis of studies on laparoscopic versus liver resection focusing on long term outcome and analyzing differently the HCC and the colorectal liver metastases patients found no differences in the 1-, 3- or 5-year survival rates (38). The international consensus conference on laparoscopic liver surgery suggested that laparoscopic surgery does not change the indications for surgery and its primary indication of laparoscopic procedures are single lesions 5 cm or less in peripheral segments recognizing the important of significant experience for extensive operations (82).
It cannot be emphasized enough that these reports of LLR come from high-volume, specialized centers and surgeons with significant experience both in open and laparoscopic surgery and the ability to choose laparoscopic surgery when it can be done safely and effectively.
Even fewer data exist about robotic liver resections (RLR) for HCC. Robotic surgery is associated with some intrinsic benefits which are visual (3-dimensional view, improved depth of perception, magnification capability) and technical (articulating instruments, degrees of freedom, tremor filtration) (83). In the few existing case series in appears to be equally effective with open and laparoscopic surgery with some authors supporting that it allows for better suturing in confined spaces, facilitating demanding procedures such as biliary reconstruction (84). Even though the existing data are limited to small case series it is important to emphasize that the existing series come from experienced surgeons and highly selected patients and tumors and are not generalizable at present. In a recent review of robotic surgery for oncologic surgery it was shown that robotic surgery is widely used for variety of operations and for several procedures, there is evidence that robotics offer short-term benefits with comparable safety profiles and oncologic outcomes (85). However, long-term oncologic outcomes are generally lacking, and robotic surgeries are more costly than open or laparoscopic surgeries. Prospective, randomized, comparative studies are needed before any statements can be made.
Summary and future perspectives
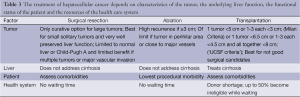
Curative treatment of hepatocellular carcinoma is particularly challenging because it should incorporate a variety of factors related to the tumor stage (size, number, location, vascular involvement), the underlying hepatic reserve (cirrhosis early vs. late), the patient’s medical comorbidities as well as the available resources which might be country specific or even hospital specific.
Surgical advances have enabled transplantation for patients with more advanced tumors and underlying liver disease. Pre-transplant therapy coupled with a surveillance period is increasingly being used in order to select the appropriate candidates for such an approach. At the same time surgical resection has entered a minimally invasive era with its inherent advantages and challenges.
Multiple risk stratification schemes exist in an attempt to assess risk and better select patients. One should also be aware that tumor clinical characteristics might be weighed differently by transplant vs. non-transplant surgeons (86).
Therefore, a multidisciplinary team, involving surgeons, hepatologists, oncologists, interventional and diagnostic radiologists, and pathologists is the most effective way to tailor the treatment plan to an individual patient’s characteristics and to the available resources and experience (Table 3).
Full table
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Fong Y, Sun RL, Jarnagin W, et al. An analysis of 412 cases of hepatocellular carcinoma at a Western center. Ann Surg 1999;229:790-9; discussion 799-800. [PubMed]
- Altekruse SF, McGlynn KA, Reichman ME. Hepatocellular carcinoma incidence, mortality, and survival trends in the United States from 1975 to 2005. J Clin Oncol 2009;27:1485-91. [PubMed]
- Forner A, Llovet JM, Bruix J. Hepatocellular carcinoma. Lancet 2012;379:1245-55. [PubMed]
- Jarnagin W, Chapman WC, Curley S, et al. Surgical treatment of hepatocellular carcinoma: expert consensus statement. HPB (Oxford) 2010;12:302-10. [PubMed]
- Schwartz M, Roayaie S, Konstadoulakis M. Strategies for the management of hepatocellular carcinoma. Nat Clin Pract Oncol 2007;4:424-32. [PubMed]
- Llovet JM, Burroughs A, Bruix J. Hepatocellular carcinoma. Lancet 2003;362:1907-17. [PubMed]
- D’Amico G, Garcia-Tsao G, Pagliaro L. Natural history and prognostic indicators of survival in cirrhosis: a systematic review of 118 studies. J Hepatol 2006;44:217-31. [PubMed]
- Bruix J, Castells A, Bosch J, et al. Surgical resection of hepatocellular carcinoma in cirrhotic patients: prognostic value of preoperative portal pressure. Gastroenterology 1996;111:1018-22. [PubMed]
- Mazzaferro V, Regalia E, Doci R, et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med 1996;334:693-9. [PubMed]
- Yao FY, Ferrell L, Bass NM, et al. Liver transplantation for hepatocellular carcinoma: expansion of the tumor size limits does not adversely impact survival. Hepatology 2001;33:1394-403. [PubMed]
- Cucchetti A, Ercolani G, Vivarelli M, et al. Impact of model for end-stage liver disease (MELD) score on prognosis after hepatectomy for hepatocellular carcinoma on cirrhosis. Liver Transpl 2006;12:966-71. [PubMed]
- Lau H, Man K, Fan ST, et al. Evaluation of preoperative hepatic function in patients with hepatocellular carcinoma undergoing hepatectomy. Br J Surg 1997;84:1255-9. [PubMed]
- Matsumata T, Kanematsu T, Yoshida Y, et al. The indocyanine green test enables prediction of postoperative complications after hepatic resection. World J Surg 1987;11:678-81. [PubMed]
- Bismuth H, Chiche L, Adam R, et al. Liver resection versus transplantation for hepatocellular carcinoma in cirrhotic patients. Ann Surg 1993;218:145-51. [PubMed]
- Llovet JM, Fuster J, Bruix J. Intention-to-treat analysis of surgical treatment for early hepatocellular carcinoma: resection versus transplantation. Hepatology 1999;30:1434-40. [PubMed]
- Yoo HY, Patt CH, Geschwind JF, et al. The outcome of liver transplantation in patients with hepatocellular carcinoma in the United States between 1988 and 2001: 5-year survival has improved significantly with time. J Clin Oncol 2003;21:4329-35. [PubMed]
- Yao FY, Xiao L, Bass NM, et al. Liver transplantation for hepatocellular carcinoma: validation of the UCSF-expanded criteria based on preoperative imaging. Am J Transplant 2007;7:2587-96. [PubMed]
- Duffy JP, Vardanian A, Benjamin E, et al. Liver transplantation criteria for hepatocellular carcinoma should be expanded: a 22-year experience with 467 patients at UCLA. Ann Surg 2007;246:502-9; discussion 509-11. [PubMed]
- Mazzaferro V, Llovet JM, Miceli R, et al. Predicting survival after liver transplantation in patients with hepatocellular carcinoma beyond the Milan criteria: a retrospective, exploratory analysis. Lancet Oncol 2009;10:35-43. [PubMed]
- Roayaie K, Feng S. Allocation policy for hepatocellular carcinoma in the MELD era: room for improvement? Liver Transpl 2007;13:S36-43. [PubMed]
- Freeman RB, Wiesner RH, Edwards E, et al. Results of the first year of the new liver allocation plan. Liver Transpl 2004;10:7-15. [PubMed]
- Teh SH, Christein J, Donohue J, et al. Hepatic resection of hepatocellular carcinoma in patients with cirrhosis: Model of End-Stage Liver Disease (MELD) score predicts perioperative mortality. J Gastrointest Surg 2005;9:1207-15; discussion 1215. [PubMed]
- Roberts JP, Venook A, Kerlan R, et al. Hepatocellular carcinoma: Ablate and wait versus rapid transplantation. Liver Transpl 2010;16:925-9. [PubMed]
- Liapi E, Geschwind JF. Transcatheter and ablative therapeutic approaches for solid malignancies. J Clin Oncol 2007;25:978-86. [PubMed]
- Lencioni R. Loco-regional treatment of hepatocellular carcinoma. Hepatology 2010;52:762-73. [PubMed]
- Weber SM, Lee FT Jr. Expanded treatment of hepatic tumors with radiofrequency ablation and cryoablation. Oncology (Williston Park) 2005;19:27-32. [PubMed]
- Mulier S, Ni Y, Jamart J, et al. Local recurrence after hepatic radiofrequency coagulation: multivariate meta-analysis and review of contributing factors. Ann Surg 2005;242:158-71. [PubMed]
- Livraghi T, Meloni F, Di Stasi M, et al. Sustained complete response and complications rates after radiofrequency ablation of very early hepatocellular carcinoma in cirrhosis: Is resection still the treatment of choice? Hepatology 2008;47:82-9. [PubMed]
- Huang GT, Lee PH, Tsang YM, et al. Percutaneous ethanol injection versus surgical resection for the treatment of small hepatocellular carcinoma: a prospective study. Ann Surg 2005;242:36-42. [PubMed]
- Chen MS, Li JQ, Zheng Y, et al. A prospective randomized trial comparing percutaneous local ablative therapy and partial hepatectomy for small hepatocellular carcinoma. Ann Surg 2006;243:321-8. [PubMed]
- Lü MD, Kuang M, Liang LJ, et al. Surgical resection versus percutaneous thermal ablation for early-stage hepatocellular carcinoma: a randomized clinical trial. Zhonghua Yi Xue Za Zhi 2006;86:801-5. [PubMed]
- Huang J, Yan L, Cheng Z, et al. A randomized trial comparing radiofrequency ablation and surgical resection for HCC conforming to the Milan criteria. Ann Surg 2010;252:903-12. [PubMed]
- Feng K, Yan J, Li X, et al. A randomized controlled trial of radiofrequency ablation and surgical resection in the treatment of small hepatocellular carcinoma. J Hepatol 2012;57:794-802. [PubMed]
- Lim KC, Chow PK, Allen JC, et al. Systematic review of outcomes of liver resection for early hepatocellular carcinoma within the Milan criteria. Br J Surg 2012;99:1622-9. [PubMed]
- Pelletier SJ, Fu S, Thyagarajan V, et al. An intention-to-treat analysis of liver transplantation for hepatocellular carcinoma using organ procurement transplant network data. Liver Transpl 2009;15:859-68. [PubMed]
- Dutkowski P, De Rougemont O, Müllhaupt B, et al. Current and future trends in liver transplantation in Europe. Gastroenterology 2010;138:802-9.e1-4.
- Li N, Wu YR, Wu B, et al. Surgical and oncologic outcomes following laparoscopic versus open liver resection for hepatocellular carcinoma: A meta-analysis. Hepatol Res 2012;42:51-9. [PubMed]
- Parks KR, Kuo YH, Davis JM, et al. Laparoscopic versus open liver resection: a meta-analysis of long-term outcome. HPB (Oxford) 2013. [Epub ahead of print].
- Li L, Zhang J, Liu X, et al. Clinical outcomes of radiofrequency ablation and surgical resection for small hepatocellular carcinoma: a meta-analysis. J Gastroenterol Hepatol 2012;27:51-8. [PubMed]
- Cucchetti A, Piscaglia F, Cescon M, et al. Cost-effectiveness of hepatic resection versus percutaneous radiofrequency ablation for early hepatocellular carcinoma. J Hepatol 2013;59:300-7. [PubMed]
- Imai K, Beppu T, Chikamoto A, et al. Comparison between hepatic resection and radiofrequency ablation as first-line treatment for solitary small-sized hepatocellular carcinoma of 3 cm or less. Hepatol Res 2013;43:853-64. [PubMed]
- Desiderio J, Trastulli S, Pasquale R, et al. Could radiofrequency ablation replace liver resection for small hepatocellular carcinoma in patients with compensated cirrhosis? A 5-year follow-up. Langenbecks Arch Surg 2013;398:55-62. [PubMed]
- Elnekave E, Erinjeri JP, Brown KT, et al. Long-Term Outcomes Comparing Surgery to Embolization-Ablation for Treatment of Solitary HCC <7 cm. Ann Surg Oncol 2013;20:2881-6. [PubMed]
- Yan K, Chen MH, Yang W, et al. Radiofrequency ablation of hepatocellular carcinoma: long-term outcome and prognostic factors. Eur J Radiol 2008;67:336-47. [PubMed]
- Orlando A, Leandro G, Olivo M, et al. Radiofrequency thermal ablation vs. percutaneous ethanol injection for small hepatocellular carcinoma in cirrhosis: meta-analysis of randomized controlled trials. Am J Gastroenterol 2009;104:514-24. [PubMed]
- Liau KH, Ruo L, Shia J, et al. Outcome of partial hepatectomy for large (> 10 cm) hepatocellular carcinoma. Cancer 2005;104:1948-55. [PubMed]
- Omata M, Lesmana LA, Tateishi R, et al. Asian Pacific Association for the Study of the Liver consensus recommendations on hepatocellular carcinoma. Hepatol Int 2010;4:439-74. [PubMed]
- Kokudo N, Makuuchi M. Evidence-based clinical practice guidelines for hepatocellular carcinoma in Japan: the J-HCC guidelines. J Gastroenterol 2009;44 Suppl 19:119-21. [PubMed]
- Cha CH, Ruo L, Fong Y, et al. Resection of hepatocellular carcinoma in patients otherwise eligible for transplantation. Ann Surg 2003;238:315-21; discussion 321-3. [PubMed]
- Schwartz M. Liver transplantation: the preferred treatment for early hepatocellular carcinoma in the setting of cirrhosis? Ann Surg Oncol 2007;14:548-52. [PubMed]
- Poon RT, Fan ST, Lo CM, et al. Difference in tumor invasiveness in cirrhotic patients with hepatocellular carcinoma fulfilling the Milan criteria treated by resection and transplantation: impact on long-term survival. Ann Surg 2007;245:51-8. [PubMed]
- Imamura H, Matsuyama Y, Tanaka E, et al. Risk factors contributing to early and late phase intrahepatic recurrence of hepatocellular carcinoma after hepatectomy. J Hepatol 2003;38:200-7. [PubMed]
- Nagasue N, Uchida M, Makino Y, et al. Incidence and factors associated with intrahepatic recurrence following resection of hepatocellular carcinoma. Gastroenterology 1993;105:488-94. [PubMed]
- Okada S, Shimada K, Yamamoto J, et al. Predictive factors for postoperative recurrence of hepatocellular carcinoma. Gastroenterology 1994;106:1618-24. [PubMed]
- Adachi E, Maeda T, Matsumata T, et al. Risk factors for intrahepatic recurrence in human small hepatocellular carcinoma. Gastroenterology 1995;108:768-75. [PubMed]
- Baccarani U, Isola M, Adani GL, et al. Superiority of transplantation versus resection for the treatment of small hepatocellular carcinoma. Transpl Int 2008;21:247-54. [PubMed]
- Sala M, Fuster J, Llovet JM, et al. High pathological risk of recurrence after surgical resection for hepatocellular carcinoma: an indication for salvage liver transplantation. Liver Transpl 2004;10:1294-300. [PubMed]
- Majno PE, Sarasin FP, Mentha G, et al. Primary liver resection and salvage transplantation or primary liver transplantation in patients with single, small hepatocellular carcinoma and preserved liver function: an outcome-oriented decision analysis. Hepatology 2000;31:899-906. [PubMed]
- Chan AC, Chan SC, Chok KS, et al. Treatment strategy for recurrent hepatocellular carcinoma: salvage transplantation, repeated resection, or radiofrequency ablation? Liver Transpl 2013;19:411-9. [PubMed]
- Belghiti J, Cortes A, Abdalla EK, et al. Resection prior to liver transplantation for hepatocellular carcinoma. Ann Surg 2003;238:885-92; discussion 892-3. [PubMed]
- Del Gaudio M, Ercolani G, Ravaioli M, et al. Liver transplantation for recurrent hepatocellular carcinoma on cirrhosis after liver resection: University of Bologna experience. Am J Transplant 2008;8:1177-85. [PubMed]
- Hu Z, Wang W, Li Z, et al. Recipient outcomes of salvage liver transplantation versus primary liver transplantation: a systematic review and meta-analysis. Liver Transpl 2012;18:1316-23. [PubMed]
- Adam R, Azoulay D, Castaing D, et al. Liver resection as a bridge to transplantation for hepatocellular carcinoma on cirrhosis: a reasonable strategy? Ann Surg 2003;238:508-18; discussion 518-9.. [PubMed]
- Llovet JM, Bruix J, Fuster J, et al. Liver transplantation for small hepatocellular carcinoma: the tumor-node-metastasis classification does not have prognostic power. Hepatology 1998;27:1572-7. [PubMed]
- Llovet JM, Fuster J, Bruix J, et al. The Barcelona approach: diagnosis, staging, and treatment of hepatocellular carcinoma. Liver Transpl 2004;10:S115-20. [PubMed]
- Chapman WC, Majella Doyle MB, Stuart JE, et al. Outcomes of neoadjuvant transarterial chemoembolization to downstage hepatocellular carcinoma before liver transplantation. Ann Surg 2008;248:617-25. [PubMed]
- Yao FY, Kerlan RK Jr, Hirose R, et al. Excellent outcome following down-staging of hepatocellular carcinoma prior to liver transplantation: an intention-to-treat analysis. Hepatology 2008;48:819-27. [PubMed]
- Llovet JM, Mas X, Aponte JJ, et al. Cost effectiveness of adjuvant therapy for hepatocellular carcinoma during the waiting list for liver transplantation. Gut 2002;50:123-8. [PubMed]
- Lesurtel M, Müllhaupt B, Pestalozzi BC, et al. Transarterial chemoembolization as a bridge to liver transplantation for hepatocellular carcinoma: an evidence-based analysis. Am J Transplant 2006;6:2644-50. [PubMed]
- Mazzaferro V, Battiston C, Perrone S, et al. Radiofrequency ablation of small hepatocellular carcinoma in cirrhotic patients awaiting liver transplantation: a prospective study. Ann Surg 2004;240:900-9. [PubMed]
- Freeman RB, Edwards EB, Harper AM. Waiting list removal rates among patients with chronic and malignant liver diseases. Am J Transplant 2006;6:1416-21. [PubMed]
- Yao FY, Ferrell L, Bass NM, et al. Liver transplantation for hepatocellular carcinoma: comparison of the proposed UCSF criteria with the Milan criteria and the Pittsburgh modified TNM criteria. Liver Transpl 2002;8:765-74. [PubMed]
- Yao FY, Bass NM, Nikolai B, et al. A follow-up analysis of the pattern and predictors of dropout from the waiting list for liver transplantation in patients with hepatocellular carcinoma: implications for the current organ allocation policy. Liver Transpl 2003;9:684-92. [PubMed]
- Pomfret EA, Washburn K, Wald C, et al. Report of a national conference on liver allocation in patients with hepatocellular carcinoma in the United States. Liver Transpl 2010;16:262-78. [PubMed]
- Fisher RA, Kulik LM, Freise CE, et al. Hepatocellular carcinoma recurrence and death following living and deceased donor liver transplantation. Am J Transplant 2007;7:1601-8. [PubMed]
- Grant RC, Sandhu L, Dixon PR, et al. Living vs. deceased donor liver transplantation for hepatocellular carcinoma: a systematic review and meta-analysis. Clin Transplant 2013;27:140-7. [PubMed]
- Cherqui D, Laurent A, Tayar C, et al. Laparoscopic liver resection for peripheral hepatocellular carcinoma in patients with chronic liver disease: midterm results and perspectives. Ann Surg 2006;243:499-506. [PubMed]
- Nguyen KT, Gamblin TC, Geller DA. World review of laparoscopic liver resection-2,804 patients. Ann Surg 2009;250:831-41. [PubMed]
- Chen HY, Juan CC, Ker CG. Laparoscopic liver surgery for patients with hepatocellular carcinoma. Ann Surg Oncol 2008;15:800-6. [PubMed]
- Tranchart H, Di Giuro G, Lainas P, et al. Laparoscopic resection for hepatocellular carcinoma: a matched-pair comparative study. Surg Endosc 2010;24:1170-6. [PubMed]
- Shi M, Guo RP, Lin XJ, et al. Partial hepatectomy with wide versus narrow resection margin for solitary hepatocellular carcinoma: a prospective randomized trial. Ann Surg 2007;245:36-43. [PubMed]
- Buell JF, Cherqui D, Geller DA, et al. The international position on laparoscopic liver surgery: The Louisville Statement, 2008. Ann Surg 2009;250:825-30. [PubMed]
- Ji WB, Wang HG, Zhao ZM, et al. Robotic-assisted laparoscopic anatomic hepatectomy in China: initial experience. Ann Surg 2011;253:342-8. [PubMed]
- Giulianotti PC, Coratti A, Sbrana F, et al. Robotic liver surgery: results for 70 resections. Surgery 2011;149:29-39. [PubMed]
- Yu HY, Friedlander DF, Patel S, et al. The current status of robotic oncologic surgery. CA Cancer J Clin 2013;63:45-56. [PubMed]
- Nathan H, Bridges JF, Schulick RD, et al. Understanding surgical decision making in early hepatocellular carcinoma. J Clin Oncol 2011;29:619-25. [PubMed]


