Current status of hepatocellular carcinoma in the United States
Hepatocellular carcinoma (HCC) represents a challenging malignancy of worldwide importance and is the third most common cause of cancer-related death globally (1). While most of the burden of HCC is borne in Southeast Asia, particularly China, and sub-Saharan Africa, there has been several interesting trends of HCC in the United States in the past decades. First, the latest epidemiology study has shown that the incidence rates for HCC in the United States have been rising (2,3). Second, early diagnosis of HCC continues to be challenging and most patients would present with unresectable or metastatic disease. Third, the management of HCC is evolving with many new treatment modalities applied in clinical practice. In this review, the author will highlight the key trends and current status of HCC in the United States.
Epidemiology
While the incidence of HCC in Asia is starting to plateau or decrease (4), it is increasing in the US (2,3). In 2013, HCC and intrahepatic cholangiocarcinoma have risen to become the fifth cancer related mortality in men and ninth in women in the States (5) (Table 1). Based on the SEER data, age-adjusted HCC incidence rates tripled between 1975 and 2005 (6,7). The greatest proportional increase in cases of HCC has been seen among Hispanics and whites between 45 and 60 years of age. It is worth noting that while most cancer related mortality is decreasing in the States, deaths from HCC in the US are increasing and at a rate faster than deaths from any other types of cancer (8).
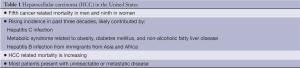
Full table
What contributes to the recent rising incidence of HCC in the United States? In contrast to the endemic regions in Southeast Asia and sub-Saharan Africa where hepatitis B (HBV) infection is responsible for the majority of HCC, chronic hepatitis C (HCV) infection is the major driver to account for the increased incidence of HCC in the States. It is estimated that approximately 4.1 million people in the United States are infected with HCV (9). In comparison to HBV, HCV causes more severe liver inflammation. Approximately 70-80% HCV-infected patients will develop chronic HCV infection and 15-20% will eventually develop cirrhosis. Once cirrhosis develops, HCC will develop at a rate of 1-4% per year. The estimated risk of HCC is 15-20 times as high among HCV-infected patients compared with those who are not HCV-infected, and the risk is largely related to those with advanced hepatic fibrosis or cirrhosis. HCV infection occurred in large numbers of young adults in North America in the 1960s and 1970s, as a result of sharing contaminated needles by users of injection drugs and from blood transfusions. HCV infection can be found in up to 30% to 50% of patients with HCC in the United States. Judging from the epidemiology trend of HCV related HCC in Japan, it has been projected that cases of HCV-related HCC will continue to increase in the United States over the next two to three decades. Alcohol is another important risk factor for HCC and a cofactor in patients with HCV infection.
Worldwide, HBV infection is responsible for the majority of HCC. It is important to appreciate that HBV vaccine is available and primary prevention through HBV vaccination is a feasible strategy to prevent HCC development. The success of this approach was first demonstrated by the nationwide Taiwanese vaccination program against HBV, which showed decreased incidence of HCC in children and the extended benefit into early adulthood (10). In the States, HBV infection in Asian and African immigrants deserves attention. The number of immigrants from Asia and Africa may contribute to the HCC incidence in large cities in the States and these patients should receive HBV vaccination and anti-HBV treatment timely.
In the States, about 20-40% of HCC patients do not have underlying HBV/HCV infection or alcohol, suggesting the presence of other causes of HCC. Some of these patients were more likely to have metabolic syndrome related to obesity, diabetes mellitus, and non-alcoholic fatty liver disease (NAFLD) (11). Given the high prevalence of the metabolic syndrome in the United States, even small increases in HCC risk related to obesity or diabetes could translate into a large number of cases of HCC, which will likely have significant impact on the trend of HCC incidence in the States in the coming decades (11). In population based cohort studies in the States, HCC was 1.5-2.0 times as likely to develop in obese persons as in those who were not obese (12). Case control and cohort studies have shown that HCC is twice as likely to develop in patients with type 2 diabetes as compared with those who do not have diabetes (13,14). Despite the clinical suspicion, there is a paucity of data supporting the direct link between progression of NAFLD and HCC development. Therefore, this potential correlation between metabolic syndrome/NAFLD and HCC warrants further investigation.
Diagnosis
Diagnosis of HCC can be rendered relatively easily in the right clinical setting for patients with well-defined risk factors, the presence of cirrhosis, and characteristic imaging findings on CT scan or liver MRI. These coupled with the use of serum alpha-fetoprotein (AFP), judicial use of biopsy, and careful interpretation of pathology will lead to the diagnosis of HCC in most cases. In patients with cirrhosis and a focal hepatic lesion larger than 2 cm in diameter, the diagnosis can be established with confidence on the basis of the presence of typical imaging features showing areas of early arterial enhancement and delayed washout in the venous or delayed phase of four-phase multidetector CT (the four phases are unenhanced, arterial, venous, and delayed) or in dynamic contrast-enhanced MRI. For lesions 1-2 cm in diameter, concordant findings from CT and MRI are recommended in order to diagnose HCC with confidence. In the United States, the guidelines for making HCC diagnosis with non-invasive methods are the same as in Europe or Asia (15). However, in the United States, tissue diagnosis with liver biopsy is performed more often than other regions in the world. Obtaining tissue diagnosis has several advantages. First, despite the strong clinical suspicion, the distinction between HCC and intrahepatic cholangiocarcinoma or the mixed HCC-cholangiocarcinoma is not always straightforward, as a result, up to 10-20% patients could be misdiagnosed. Second, other primary liver tumors or metastatic disease, or benign lesions could be the underlying diagnosis. Third, when patients present with metastatic disease, the radiologic features may not be very characteristic. Finally, tissue diagnosis will provide the critical material for molecular testing, which will potentially provide useful information in the era of personalized medicine. AFP is the most commonly used serum biomarker in the United States. Despite the wide use of des-gamma carboxy prothrombin (DCP) and lectin-bound AFP (AFP-L3) in other regions of the world (16), they are not routinely used in clinical practice in most centers in the United States.
Despite the availability of well established diagnostic tests, it remains challenging to diagnose HCC at early stage in the United States. As a result, most patients will present with unresectable or metastatic disease. This is particularly true for certain racial/ethnic groups (17) and in patients with NAFLD or no clear underlying risk factors (18). For reasons outlined above, tissue diagnosis should be obtained more often both for diagnostic purpose and for research related issues.
Staging
The heterogeneity of HCC, contributed by various factors including tumor burden, the presence and severity of underlying cirrhosis and performance status, contributes to the complexity of patient care and evaluation (19). Staging systems are useful for stratification of patients based on their prognosis prior to treatment, allocating specific treatment based on the stage, and allowing comparison of clinical outcomes from different clinical studies. Although many different staging systems have been developed, which include Barcelona Clinic Liver Cancer (BCLC) (20), Cancer of the Liver Italian Program (CLIP) (21), tumor-node-metastasis (TNM) (22), Groupe d’Etude et de Traitement du Carcinome Hépatocellulaire (GRETCH) (23), Chinese University Prognostic Index (CUPI) (24), and Japanese Integrated Staging (JIS) (25), there is currently no universally accepted staging system. The BCLC staging classification is increasingly used in the United States and it has tried to capture the tumor features, severity of cirrhosis, performance status, and a recommended treatment algorithm for each stage. However, due to the geographic variation of different risk factors, one staging system may perform better than others in certain regions. In addition, depending on the stage of the disease, certain staging system may be more prognostic, as suggested by a study comparing the various staging systems for patients with advanced disease (26). In this study, the BCLC system was found to be less informative than the GRETCH and CLIP classifications (26). In the United States, TNM, BCLC and CLIP represent some of the more commonly used staging systems. Currently, there are a lot of research and efforts trying to incorporate molecular classification into the existing staging systems (27).
Management
There are several interesting trends for the management of HCC in the United States in the past decade (Table 2). First, there are continued efforts refining the indications for surgical resection and liver transplant and to develop new surgical techniques. Second, novel local and regional liver directed therapies are being developed and increasingly applied in clinical practice. Third, following the successful approval of sorafenib, there have been renewed and ongoing interests and active efforts developing other molecularly targeted agents in this disease. Fourth, multidisciplinary management of HCC has become the theme for patient care in most hospitals in the United States.
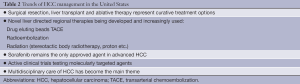
Full table
Curative treatments: surgery, transplantation, ablative therapy
Surgical resection remains the curative treatment choice for patients with resectable HCC and adequately preserved liver function. Major resections can only be performed with low rates of life-threatening complications in non-cirrhotic patients. By contrast in cirrhotic patients this procedure requires well-defined selection criteria (solitary tumors and Child-Pugh’s A patients without portal hypertension) and a skilled surgical team. In these cases, perioperative mortality should be below 3%, blood transfusion requirements of less than 10%, and 5-year survival rates of at least 50-60%. In the United States, liver resection tends to be performed by experienced surgeons specialized in hepatobiliary surgeries in major medical centers. The experience of laparoscopic resection of HCC has been expanding. In general, the laparoscopic resection is only applicable to selected patients and it may have better postoperative quality of life than those with open resection.
Tumor recurrence complicates 50-80% of cases, and there is no established standard adjuvant therapy. More than 15 randomized controlled trials (RCTs) assessing loco-regional and systemic therapies have been published including chemoembolization, internal radiation, chemotherapy or adoptive immunotherapy, retinoids or interferon. Despite the early evidence of efficacy signal such as internal radiation with 131-I-labelled lipiodol, retinoids or adoptive immunotherapy, these results were not confirmed in large randomized phase III trials and the strength of evidence was not convincing enough to become the standard of care. As a result, patients will be observed for surveillance after surgical resection without additional adjuvant therapy. In the United States, many centers and investigators have participated in the phase III randomized trial evaluating sorafenib as adjuvant therapy in the prevention of recurrence of HCC (STORM). This study has completed the enrollment of the targeted more than 1,000 patients and the results are eagerly awaited.
Liver transplantation is the first treatment choice for patients with single HCC ≤5 cm or up to three nodules each ≤3 cm or those with advanced liver dysfunction. When these criteria are met, transplant would achieve 70% survival at 5-year with a recurrence rate below 15% (28). Due to the scarcity of donors up to 10-20% of the candidates would dropout from the waiting list before receiving the procedure. Bridging therapy using either radiofrequency ablation (RFA) or transarterial chemoembolization (TACE) are commonly used in the States, however, none of the treatments applied whilst on the waiting list have been tested in the setting of randomized investigations.
Although the Milan criteria is the generally accepted standard criteria in the States, attempts to assess the transplant outcomes in patients who exceeded the Milan criteria has been explored. Other criteria including UCSF criteria have been used in selective centers in the States (29). In the States, cadaver transplant is more common than living donor transplant. Genomic translational studies enabling the identification of the best candidates based on molecular profiles are currently conducted in the States, and might better define the ideal subpopulations.
Several local ablative treatment options exist. Generally, RFA and percutaneous ethanol injection (PEI) are more commonly used to treat small HCCs that are either solitary or a few lesions. Complete responses are achieved in more than 80% of tumors smaller than 3 cm in diameter, but in 50% of tumors of 3-5 cm in size. In the United States, there is a general agreement in that RFA provides better local control of the disease as compared with PEI as shown previously (30), and thus is considered the treatment of choice. Other ablative treatment modalities including microwave ablation and irreversible electroporation (IRE) are also being tested in many centers in the States.
Liver directed regional treatment
Patients at intermediate stages of this disease present a natural outcome of 16 months of median survival (31). Chemoembolization is generally used in patients with multifocal or unresectable HCC without portal vein invasion and can improve median survival to up to 20 months in selected patients based on two randomized studies and a systematic review of six RCT (31-33). In the United States, TACE is also often used in patients with multifocal HCC and segmental portal vein thrombosis despite the lack of level 1 evidence. The added value of doxorubicin in TACE remains controversial as suggested by a randomized single blind controlled trial comparing beads versus doxorubicin-eluting beads for HCC (34).
It is encouraging that many other local treatment modalities have been explored in HCC including intra-arterial injection of Yttrium-90 microspheres, drug-eluting beads and external bema radiation in the United States. Many centers have expanded on the initial clinical experience of radioembolization with Yttrium 90 microspheres (35). Encouraged by the initial experience in Asia with liver radiation, many centers are exploring the use of radiation (SBRT, protons etc.) to the liver in the States (36). How these different local treatment approaches would compare with TACE and whether each technique will find its unique application in selected patient populations remain to be determined with randomized studies.
Perhaps the most active area of clinical research in local regional therapy in HCC in the States is the ongoing efforts combining sorafenib or other targeted agents with TACE, radioembolization or radiation. In parallel with the efforts worldwide, many investigators in the States have conducted the initial studies testing the tolerability, safety and early evidence of efficacy of sorafenib with TACE (37). Currently, ECOG 1208, a randomized phase III study assessing the combination of sorafenib or placebo with DEB-TACE in HCC, is ongoing in the United States.
Systemic treatment
In a landmark international, phase III, placebo-controlled Sorafenib HCC Assessment Randomized Protocol (SHARP) trial, sorafenib demonstrated improved OS and time to tumor progression (TTP) compared with placebo (38). Median OS was 10.7 months in the sorafenib group and 7.9 months in the placebo group (hazard ratio for the sorafenib group, 0.69; P<0.001). Based on these results, sorafenib is the only approved agent in advanced HCC in the States. As sorafenib is gaining more clinical experience, several important pictures have emerged. First, the clinical benefits are still modest and transient. This highlights the importance of understanding the mechanism of action of sorafenib and identification of predictive markers. Second, sorafenib related toxicities including hand and foot skin reaction, diarrhea, and fatigue need to be carefully monitored and timely managed. Third, since the agent was tested only in patients with underlying Child A cirrhosis in the registration trials, the benefits of sorafenib in patients with worsening hepatic dysfunction remains uncertain.
In the United States, there are active clinical trial efforts in various settings. For patients for newly diagnosed advanced HCC, current clinical studies are assessing the role of sorafenib in combination with other targeted agents or chemotherapy in advanced HCC. CALGB80802, a phase III randomized study of sorafenib plus doxorubicin versus sorafenib in patients with advanced HCC, is ongoing in an attempt to assess the added value of doxorubicin when combined with sorafenib (39). Many molecularly targeted agents are being tested in patients with advanced HCC who failed or could not tolerate sorafenib. There are also significant efforts testing novel agents in phase I trials in HCC in the States. Despite the failure of several phase III trials in the past few years, these vigorous clinical trial efforts will hopefully lead to additional approved agents in this challenging disease.
In conclusion, HCC has emerged as an important malignancy in the United States with rising incidence and high mortality. The development in all forefronts including prevention, surveillance, early diagnosis, and more effective treatment for patients with different stages of disease holds promise to further improve the outcomes for patients with HCC. Given the complexity of HCC, multidisciplinary team efforts are critical to optimize the care of HCC and have become the main theme of care in the United States. While more molecularly targeted agents are under active investigation in HCC (40), it is important to identify more relevant therapeutic targets based on our further understanding of hepatocarcinogenesis and molecular classification, to optimize the trial design and patient resources, and to develop and validate surrogate and predicative molecular markers.
Acknowledgements
Disclosure: The author declares no conflict of interest.
References
- Parkin DM, Bray F, Ferlay J, et al. Global cancer statistics, 2002. CA Cancer J Clin 2005;55:74-108. [PubMed]
- El-Serag HB, Mason AC. Rising incidence of hepatocellular carcinoma in the United States. N Engl J Med 1999;340:745-50. [PubMed]
- El-Serag HB, Davila JA, Petersen NJ, et al. The continuing increase in the incidence of hepatocellular carcinoma in the United States: an update. Ann Intern Med 2003;139:817-23. [PubMed]
- Kim SR, Kudo M, Hino O, et al. Epidemiology of hepatocellular carcinoma in Japan and Korea. A review. Oncology 2008;75 Suppl 1:13-6. [PubMed]
- Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin 2013;63:11-30. [PubMed]
- El-Serag HB. Hepatocellular carcinoma. N Engl J Med 2011;365:1118-27. [PubMed]
- Altekruse SF, McGlynn KA, Reichman ME. Hepatocellular carcinoma incidence, mortality, and survival trends in the United States from 1975 to 2005. J Clin Oncol 2009;27:1485-91. [PubMed]
- Jemal A, Siegel R, Ward E, et al. Cancer statistics, 2009. CA Cancer J Clin 2009;59:225-49. [PubMed]
- Armstrong GL, Wasley A, Simard EP, et al. The prevalence of hepatitis C virus infection in the United States, 1999 through 2002. Ann Intern Med 2006;144:705-14. [PubMed]
- Chang MH, Chen CJ, Lai MS, et al. Universal hepatitis B vaccination in Taiwan and the incidence of hepatocellular carcinoma in children. Taiwan Childhood Hepatoma Study Group. N Engl J Med 1997;336:1855-9. [PubMed]
- Siegel AB, Zhu AX. Metabolic syndrome and hepatocellular carcinoma: two growing epidemics with a potential link. Cancer 2009;115:5651-61. [PubMed]
- Calle EE, Rodriguez C, Walker-Thurmond K, et al. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med 2003;348:1625-38. [PubMed]
- El-Serag HB, Hampel H, Javadi F. The association between diabetes and hepatocellular carcinoma: a systematic review of epidemiologic evidence. Clin Gastroenterol Hepatol 2006;4:369-80. [PubMed]
- El-Serag HB. Hepatocellular carcinoma: recent trends in the United States. Gastroenterology 2004;127:S27-34. [PubMed]
- European Association For The Study Of The Liver, European Organisation For Research And Treatment Of Cancer. EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol 2012;56:908-43. [PubMed]
- Volk ML, Hernandez JC, Su GL, et al. Risk factors for hepatocellular carcinoma may impair the performance of biomarkers: a comparison of AFP, DCP, and AFP-L3. Cancer Biomark 2007;3:79-87. [PubMed]
- Sloane D, Chen H, Howell C. Racial disparity in primary hepatocellular carcinoma: tumor stage at presentation, surgical treatment and survival. J Natl Med Assoc 2006;98:1934-9. [PubMed]
- Nascimbeni F, Pais R, Bellentani S, et al. From NAFLD in clinical practice to answers from guidelines. J Hepatol 2013;59:859-71. [PubMed]
- Marrero JA, Kudo M, Bronowicki JP. The challenge of prognosis and staging for hepatocellular carcinoma. Oncologist 2010;15 Suppl 4:23-33. [PubMed]
- Llovet JM, Brú C, Bruix J. Prognosis of hepatocellular carcinoma: the BCLC staging classification. Semin Liver Dis 1999;19:329-38. [PubMed]
- A new prognostic system for hepatocellular carcinoma: a retrospective study of 435 patients: the Cancer of the Liver Italian Program (CLIP) investigators. Hepatology 1998;28:751-5. [PubMed]
- Sobin LH. TNM, sixth edition: new developments in general concepts and rules. Semin Surg Oncol 2003;21:19-22.
- Chevret S, Trinchet JC, Mathieu D, et al. A new prognostic classification for predicting survival in patients with hepatocellular carcinoma. Groupe d’Etude et de Traitement du Carcinome Hépatocellulaire. J Hepatol 1999;31:133-41. [PubMed]
- Leung TW, Tang AM, Zee B, et al. Construction of the Chinese University Prognostic Index for hepatocellular carcinoma and comparison with the TNM staging system, the Okuda staging system, and the Cancer of the Liver Italian Program staging system: a study based on 926 patients. Cancer 2002;94:1760-9. [PubMed]
- Kudo M, Chung H, Osaki Y. Prognostic staging system for hepatocellular carcinoma (CLIP score): its value and limitations, and a proposal for a new staging system, the Japan Integrated Staging Score (JIS score). J Gastroenterol 2003;38:207-15. [PubMed]
- Huitzil-Melendez FD, Capanu M, O’Reilly EM, et al. Advanced hepatocellular carcinoma: which staging systems best predict prognosis? J Clin Oncol 2010;28:2889-95. [PubMed]
- Kaseb AO, Morris JS, Hassan MM, et al. Clinical and prognostic implications of plasma insulin-like growth factor-1 and vascular endothelial growth factor in patients with hepatocellular carcinoma. J Clin Oncol 2011;29:3892-9. [PubMed]
- Mazzaferro V, Regalia E, Doci R, et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med 1996;334:693-9. [PubMed]
- Yao FY, Ferrell L, Bass NM, et al. Liver transplantation for hepatocellular carcinoma: expansion of the tumor size limits does not adversely impact survival. Hepatology 2001;33:1394-403. [PubMed]
- Lencioni RA, Allgaier HP, Cioni D, et al. Small hepatocellular carcinoma in cirrhosis: randomized comparison of radio-frequency thermal ablation versus percutaneous ethanol injection. Radiology 2003;228:235-40. [PubMed]
- Llovet JM, Bruix J. Systematic review of randomized trials for unresectable hepatocellular carcinoma: Chemoembolization improves survival. Hepatology 2003;37:429-42. [PubMed]
- Llovet JM, Real MI, Montaña X, et al. Arterial embolisation or chemoembolisation versus symptomatic treatment in patients with unresectable hepatocellular carcinoma: a randomised controlled trial. Lancet 2002;359:1734-9. [PubMed]
- Lo CM, Ngan H, Tso WK, et al. Randomized controlled trial of transarterial lipiodol chemoembolization for unresectable hepatocellular carcinoma. Hepatology 2002;35:1164-71. [PubMed]
- Brown KT, Gonen M, Do KG, et al. A randomized single blind controlled trial of beads versus doxorubicin-eluting beads for arterial embolization of hepatocellular carcinoma (HCC). J Clin Oncol 2012;30:abstr 143.
- Kulik LM, Carr BI, Mulcahy MF, et al. Safety and efficacy of 90Y radiotherapy for hepatocellular carcinoma with and without portal vein thrombosis. Hepatology 2008;47:71-81. [PubMed]
- Tse RV, Hawkins M, Lockwood G, et al. Phase I study of individualized stereotactic body radiotherapy for hepatocellular carcinoma and intrahepatic cholangiocarcinoma. J Clin Oncol 2008;26:657-64. [PubMed]
- Pawlik TM, Reyes DK, Cosgrove D, et al. Phase II trial of sorafenib combined with concurrent transarterial chemoembolization with drug-eluting beads for hepatocellular carcinoma. J Clin Oncol 2011;29:3960-7. [PubMed]
- Llovet JM, Ricci S, Mazzaferro V, et al. Sorafenib in advanced hepatocellular carcinoma. N Engl J Med 2008;359:378-90. [PubMed]
- Abou-Alfa GK, Johnson P, Knox JJ, et al. Doxorubicin plus sorafenib vs doxorubicin alone in patients with advanced hepatocellular carcinoma: a randomized trial. JAMA 2010;304:2154-60. [PubMed]
- Zhu AX. Molecularly targeted therapy for advanced hepatocellular carcinoma in 2012: current status and future perspectives. Semin Oncol 2012;39:493-502. [PubMed]


