Neoadjuvant chemoradiotherapy followed by surgery for stage IIIa and IIIb non-small-cell lung cancer (NSCLC): is it still justified?
Introduction
Neo-adjuvant or preoperative therapy for operable non-small-cell lung cancer (NSCLC) has been the subject of a large number of studies in the literature, and in spite of progress demonstrated by well conceived and well conducted phase III randomized trials and meta-analyses, many issues remain unsolved as of today, especially in locally advanced (LA) stages. In operable stage III NSCLC, there is still a considerable debate regarding the best strategy, which can include surgery followed by chemotherapy with or without radiotherapy, neo-adjuvant chemotherapy followed by surgery with or without post-operative radiotherapy, neo-adjuvant chemoradiation followed by surgery, comprehensive chemoradiation without surgery, proceeded or not by neo-adjuvant chemotherapy, and several other strategies (1,2). Neo-adjuvant treatments are aimed at improving the overall outcome of LA NSCLC by decreasing the rate of local failures and distant metastases observed after surgery alone.
After a brief reminder on the role of neo-adjuvant chemotherapy in NSCLC, this article will focus in more details on the potential added value of radiotherapy in the neoadjuvant setting.
Neoadjuvant chemotherapy in LA NSCLC
In non-metastatic NSCLC surgery still represents the mainstay of curative treatments from stage IA to IIIA and even for part of stage IIIB. However, especially in LA NSCLC, overall survival after surgery alone remains poor, in the range of 5–10% at 5 years (3). The domain of neo-adjuvant or adjuvant chemotherapy spans from stage IB to part of stage IIIB (4-8), due to the subsequent high risk of distant metastases after surgery alone.
The recent meta-analysis on neo-adjuvant chemotherapy for NSCLC has collected individual participant data from 2,385 patients included in 15 controlled randomized trials (4). Patients were centrally analyzed, and the primary outcome was overall survival. The results showed a 13% reduction in the relative risk of death, with an absolute survival improvement of 5% at 5 years, from 40% to 45% (4). In this meta-analysis, stage did not seem to alter the effect of chemotherapy. Looking at the first events, local recurrence occurred in 24%, distant recurrence in 31% and both local and distant recurrence in 9%. Altogether 33% of first events included a local failure (4). In a previous meta-analysis, which was not based on individual patient’s data, the positive effect of chemotherapy was also observed, and looking specifically at 8 studies on stage III, the improvement in overall survival with chemotherapy remained statistically significant (5). However neo-adjuvant chemotherapy alone in stage III may not be sufficient, since even with this approach, the pathological complete response (pCR) rate was low, and the local-regional recurrence rate was high. For example, in three randomized trials comparing neo-adjuvant chemotherapy followed by surgery to surgery alone in stage III NSCLC, the complete pCR in the induction arm was only between 6% and 10.5% (6-8). As pCR is an indicator of response and a possible surrogate for survival (see below), it seems logical to improve pCR by an additional local treatment to surgery such as radiation therapy. In a phase II trial of the Swiss cooperative group (SAKK), in which patients received neo-adjuvant docetaxel and cisplatin for stage IIIA NSCLC, there was a good correlation between pathological response and resectability; in addition, resectability and mediastinal clearance were strongly prognostic for survival, whereas patients with no mediastinal clearing and/or an incomplete resection did poorly (9). A subsequent analysis of this phase II revealed that at 5-year follow-up, as many as 60% of patients suffered from a local relapse (10). For these different reasons, it appears that the addition of radiotherapy to chemotherapy in neo-adjuvant strategies deserves to be strongly considered.
Neoadjuvant radiochemotherapy in LA NSCLC: retrospective studies, database and phase II trials
Retrospective studies
A large number of retrospective studies on neo-adjuvant radiochemotherapy for stage III NSCLC have been published. The overall results of a selection of eight of these are briefly discussed here (11-18). They represent altogether a total of about 1,100 patients with operable stage IIIA and IIIB (11-18). In the majority, chemotherapy consisted of cisplatin doublets, with a few carboplatin doublets, and the radiotherapy schedules were mainly conventional fractionation schemes with a few hyperfractionated schemes, with doses between 43 and 60 Gy. The pCR, when reported, varied between 16% and 27% (11,13-15,18), except in one study where it was as high as 40% (17). The median survival was between 21 and 36 months, and the 5-year overall survival between 31% and 40% (11-18). In several reports, a pCR was associated with an increased survival (11,12,17,18), and a mediastinal downstaging and/or pathological clearing was also heralding a superior outcome (12-14,16,17). Evidently, results from these retrospective studies are to be interpreted with caution due to patients‘ selection and other bias. However some striking results, like the rates of pCR and the relationship between pCR, downstaging and survival are encouraging and may be hypothesis-forming for prospective randomized trials.
Results of the American National Cancer Database (NCDB)
A cohort of 11,242 patients included in the NCDB, treated from 1998 to 2004 for stage IIIA (N2) NSCLC were analyzed according to the 5 following treatment categories: neoadjuvant chemoradiation followed by a lobectomy, neo-adjuvant chemoradiation followed by pneumonectomy, lobectomy followed by adjuvant treatment, pneumonectomy followed by adjuvant treatment, or concomitant chemoradiation without surgery (19). Adjuvant treatments consisted of either chemotherapy alone, radiotherapy alone, or chemoradiation following surgery. Five-year overall survival was 33.5%, 20.7%, 20.3%, 13.3%, and 10.9%, respectively for the five treatment categories (19). On multivariate analysis, the hazard ratio (HR) in favor of the neo-adjuvant chemoradiation treatment was 0.51 (CI: 0.45–0.58) (19). Of note however, no neo-adjuvant chemotherapy alone category was described in this report. A more recent study from the NCDB analyzed 1,076 patients with stage IIIA (N2) NSCLC, treated between 2003 to 2005, either with neo-adjuvant chemoradiation followed by surgery or neoadjuvant chemotherapy followed by surgery (20). Outcomes included overall survival, residual nodal disease, any adverse pathologic features, and 30-day postoperative mortality. The 5-year overall survival for the entire cohort was 39%, namely 39.2% for the neo-adjuvant chemoradiation category vs. 38.6% for the neo-adjuvant chemotherapy (P= NS). On multivariate analysis, neo-adjuvant chemoradiation was associated with an improved pathological outcome (20).
Phase II trials
Results of 7 selected prospective one-arm phase II studies are presented on Table 1 (21-27). In 5 of these trials, there was a mixture of stage IIIA and IIIB, whereas 2 have included stage IIIB only (22,25). In all studies, chemotherapy consisted of cisplatin doublets or carboplatin doublets. All trials but one (25) included a concomitant chemoradiotherapy regimen, and radiotherapy schedules delivered doses between 40 and 50.4 Gy, except for one in which a hyperfractionated scheme of 69.6 Gy was administered (23). Surgical results showed a resectability rate between 62% and 93%, with a post-operative mortality between 0% and 8%. pCR, looking at the surgical specimen of the primary tumor, was reported to be between 13% and 44%. Median survival was between 13 and 29.6 months, and 3-year survival between 24% and 64%. When overall survivals of stage IIIA and IIIB were compared, there was no difference (21,26). This most likely reflected a favorable selection of operable stage IIIB patients, but at the same time it indicated that at least a subset of stage IIIB patients could benefit from neoadjuvant chemoradiation (21,22,25,26). Finally, when reported, there was a strong correlation between complete resection (R0) and survival (25,26), mediastinal clearing and survival (21,24,25), and pCR and survival (24,25).
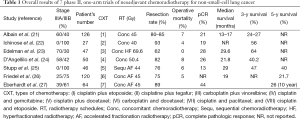
Full table
Surrogates for survival
From a number of retrospective studies and prospective phase II studies mentioned above, it appears thus than pCR, mediastinal downstaging or clearing, and R0 resection were associated with an improved survival. It should be reminded that after neoadjuvant chemotherapy alone, pCR was between 6% and 10% only in stage III, whereas it was between 16% and up to 40% in retrospective neo-adjuvant chemoradiation studies, and between 13% and 44% in phase II prospective neoadjuvant chemoradiation trials. Radiotherapy has not only the potential to improve pCR of the primary tumor, but to increase mediastinal clearing in case of N2 disease and to ameliorate the R0 resection rate. Yet its impact on survival would have to be demonstrated by phase III randomized trials only.
Neoadjuvant radiochemotherapy in LA NSCLC: prospective randomized trials
Neo-adjuvant chemoradiation followed by surgery versus neo-adjuvant chemotherapy followed by surgery and post-operative radiotherapy: the German phase III randomized German Lung Cancer Cooperative Group (GLCCG) trial (28)
The GLCCG in a large phase III trial has randomized 558 patients with stage IIIA and IIIB NSCLC into two treatment groups (28). The intervention group received three cycles of cisplatin and etoposide, followed by twice daily radiation to 45 Gy and concurrent carboplatin and vindesine, followed by surgical resection. The control group received three cycles of cisplatin and etoposide, followed by surgery, followed by postoperative radiotherapy to 54–68 Gy. Primary endpoint was progression-free survival and secondary endpoints were overall survival and resectability. Results showed no significant difference in progression-free survival (37% vs. 33%) and no difference in overall survival (39% vs. 31%) between the two groups (28). However the group with preoperative chemoradiation showed a better pathological response, defined here as >90% tumor clearing, with 60% vs. 20% (P=0.0001), and a better mediastinal downstaging, with 46% vs. 29% (P=0.002), with no difference in the occurence of treatment-related deaths (6.4% vs. 5.7%) (28).
Thus, this important trial could clearly demonstrate a greater local efficacy of chemoradiation compared to chemotherapy alone, but there was no impact on progression-free survival and overall survival. It may be that in the control group (neo-adjuvant chemotherapy alone), the systematic use post-operative radiotherapy may have «blurred» the impact of neo-adjuvant radiotherapy of the other arm. In any case, and unfortunately, this trial did not answer the question whether the addition of radiotherapy to chemotherapy in the neo-adjuvant setting improves or not the overall outcome.
Neo-adjuvant chemoradiation followed by surgery versus neo-adjuvant chemotherapy: phase II randomized (29) and incomplete phase III randomized trials (30)
A French phase II randomized study on 47 patients with stage IIIA N2 NSCLC aimed at comparing standard induction chemotherapy (arm A: cisplatin and gemcitabine), with 2 different induction chemoradiation regimens (arm B: cisplatin and vinorelbine) and radiotherapy dose: 46 Gy, arm C: carboplatin and paclitaxel and radiotherapy dose 46 Gy (29). Response rate was higher in the 2 chemoradiation arms compared to the chemotherapy only arm (87% vs. 57%, P=0.049). Feasibility rate was the same in the 3 arms, the overall survival for the entire cohort was 43% at 3 years, with no difference between the 3 arms (29). Neither the study design nor the small number of patients could allow to evaluate a possible difference in overall survival.
A Japanese phase III randomized trial for stage IIIA N2 NSCLC was sought to ascertain whether induction concurrent chemoradiation followed by surgery could improve survival compared to induction chemotherapy followed by surgery (30). Patients received either carboplatin and docetaxel plus concurrent radiation therapy to 40 Gy followed by surgery, or induction chemotherapy alone followed by surgery (30). The study had to be stopped because of slow accrual, but 60 patients could finally be randomized. Treatments were well tolerated and there was no toxic deaths. Combined chemoradiation conferred a better local control, however there was no differences in progression-free survival or overall survival when radiotherapy was added to chemotherapy (30).
Thus these two small randomized trials showed clearly a greater measurable therapeutic effect of neoadjuvant chemoradiation compared to adjuvant chemotherapy alone, but were unable to demonstrate any impact on progression-free survival or overall survival, and this was, possibly in part, due to the small numbers of patients.
Neo-adjuvant chemoradiation followed by surgery versus neo-adjuvant chemotherapy: the Swiss phase III randomized SAKK trial (31)
The Swiss cooperative group, the SAKK, in a phase III randomized trial has enrolled 232 patients with stage IIIA N2 NSCLC into two treatment groups (31). At this time, it is the only fully completed phase III randomized trial with this design. The radiochemotherapy group (117 patients) received three cycles of neoadjuvant cisplatin and docetaxel, followed by radiotherapy with 44 Gy in 22 fractions over 3 weeks. The control group (115 patients) received the same chemotherapy alone, and all patients were scheduled to undergo surgery. Primary endpoint was event-free survival. Overall tumor response rate was 61% after chemoradiation, vs. 44% after chemotherapy alone (P=0.012). Overall, chemotherapy-related effects were moderate and similar in the two groups, and radiotherapy-related toxic effects were also moderate with 9 grade 3 events (31). Eighty five percent in the chemoradiotherapy group and 82% in the chemotherapy group underwent surgery. A R0 resection was performed in 91% and 81%, respectively (P=0.06). In the 30 days after surgery, 3 patients in the chemotherapy group died, compared with none in the chemoradiotherapy group. Nodal downstaging (to N1 or N0) was observed in 64% and 53%, respectively, and the pCR in 16% and 12%, respectively in the chemoradiation group and chemotherapy only group (P= NS). The first event was death in 13% patients in the chemoradiation group vs. 8% in the chemotherapy group, and was local progression in 15% and 28%, respectively. The median event-free survival was 12.8 months in the chemoradiotherapy group and 11.6 months in the chemotherapy group (P=0.67). Median overall survival was 37.1 months in the chemoradiotherapy group, and 26.2 months in the chemotherapy group, but survivals at 2, 3 and 4 years were identical in the 2 treatment arms (31).
Thus, this study showed that patients who received chemoradiotherapy before surgery had an objective response, a pCR, a R0 resection rate and a mediastinal downstaging more frequently and less local progression than patients in the chemotherapy alone group. In spite of all of these, the addition of radiotherapy did neither improve event-free survival (the primary endpoint) nor overall survival (31). The reasons for this may have been due to several factors. Firstly radiotherapy was given sequentially to chemotherapy, and not concomitantly, whereas concomitant chemoradiation was shown in the NSCLC Collaborative Group meta-analysis to be superior to sequential schedules in LA disease (32). Secondly the radiotherapy dose (44 Gy), although given in a slightly accelerated schedule (equivalent to 48–50 Gy in conventional daily fractions of 2 Gy), may have been insufficient. These two factors may explain a pCR of 16%, which is inferior to the pCR rates observed in retrospective data and in phase II trials using concomitant schedules and/or higher RT doses (see Table 1). Other factors, including the high distant failure rates in both arms (37% and 33% rates of first relapse), the patients’ selection and the relatively small number of patients may have contributed. On the other hand, the addition of radiotherapy was well tolerated and did neither increase hematological toxicity nor post-operative mortality, which were altogether low in this trial.
Discussion
Although results from retrospective data and from phase II trials have suggested that the addition of neo-adjuvant radiotherapy to chemotherapy could improve the outcome of operable stage III NSCLC, none of the small randomized trials, including the recent SAKK trial could demonstrate any advantage in event-free, progression-free or overall survival (29-31). Does it mean that radiotherapy should be banned from the adjuvant setting in the future? At the present time, different opinions prevail:
- Pless et al. in the conclusion of their SAKK trial, have argued that in stage III NSCLC, three modalities are not superior to two modalities, and that one local treatment may be enough (31). The main reasons were that on one hand, neoadjuvant chemotherapy alone gave similar results as neoadjuvant chemoradiation in the three published randomized trials (29-31), and that on the other hand three other large randomized trials have shown that after neoadjuvant chemotherapy, either high-dose radiotherapy alone or surgery alone were equivalent in terms of overall survival (33-35);
- Eberhardt and Stuschke in an editorial commenting the results of the SAKK trial, consider that for most patients, the combination of chemotherapy and concurrent radiotherapy represents an acceptable standard (2). One of their arguments is based on their own data on intensive neoadjuvant concurrent chemoradiotherapy in which they found fairly high rates of pCR, between 30% and 40% (27,35), which were substantially higher than the 16% pCR of the SAKK study (31). They also stress that stage III disease is heterogeneous in terms of tumor volume and bulk, lymphogenic spread and co-morbidity (2). Thus, different subgroups of stage III may deserve different strategies, and personalized treatments based on co-morbidities might be a better solution (2).
Indeed, as almost all studies have shown better results with chemoradiation concerning response rate, pathological response, mediastinal clearing and local control of the disease, all of which being potential surrogates for survival, it seems justified to pursue the study of the role of concomitant chemoradiotherapy in the neoadjuvant setting, however only under certain conditions.
- Better selection of patients: one should first identify subgroups of operable stage III NSCLC who probably do not need additional RT, for example stage IIIA with minimal N2 disease, and exclude this group from radiochemotherapy trials. New trials should then be dedicated to subgroups with a higher risk of local failure, such as stage III-N2 bulky disease, stage IIIB, and superior sulcus tumors. In the latter situation in particular, neoadjuvant chemoradiation gave excellent results in phase 2 studies (36,37);
- Better radiotherapy: new trials should include innovative, high-technology radiotherapy capable of delivering safely high doses of radiation, concomitantly (and not sequentially) to chemotherapy. Techniques using intensity modulated radiotherapy (IMRT), image-guided radiotherapy (IGRT) (17), and/or adaptive radiotherapy would be essential, and schedules like accelerated fractionation (26,27), concomitant boost (35), dose-escalation or hypofractionated schemes should be worth studying;
- Better systemic treatments in combination with radiotherapy: it should be remembered that current “standard” cisplatin doublets have their limitations. The pCR and local control with currently available chemotherapy alone is low, and the rate of distant failures is still high (vide supra), indicating a limited efficacy even on microscopic disease.
In conclusion, neoadjuvant chemoradiotherapy for stage III NSCLC is safe and efficient, with higher overall clinical response, higher pCR rates and a higher mediastinal clearing compared to neoadjuvant chemotherapy alone. Contrary to previous fears, radiotherapy does not add a higher toxicity nor does it increase post-operative mortality compared to chemotherapy alone. Numerous phase II trials have shown encouraging survival rates, up to 30–40% at 5 years. On the other hand, the yet available randomized studies have failed to demonstrate any advantage of adding radiotherapy in the neoadjuvant setting regarding progression-free survival or overall survival. Admittedly the number of patients enrolled was modest. Still the controversy is not being solved and further trials taking into account a better patients’ selection, innovative radiotherapy and more efficient systemic treatments need to be undertaken.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Eberhardt WE, De Ruysscher D, Weder W, et al. 2nd ESMO Consensus Conference in Lung Cancer: locally advanced stage III non-small-cell lung cancer. Ann Oncol 2015;26:1573-88. [PubMed]
- Eberhardt WE, Stuschke M. Multimodal treatment of non-small-cell lung cancer. Lancet 2015;386:1018-20. [PubMed]
- Mountain CF. Revisions in the International System for Staging Lung Cancer. Chest 1997;111:1710-7. [PubMed]
- NSCLC Meta-analysis Collaborative Group. Preoperative chemotherapy for non-small-cell lung cancer: a systematic review and meta-analysis of individual participant data. Lancet 2014;383:1561-71. [PubMed]
- Song WA, Zhou NK, Wang W, et al. Survival benefit of neoadjuvant chemotherapy in non-small-cell lung cancer: an updated meta-analysis of 13 randomized control trials. J Thorac Oncol 2010;5:510-6. [PubMed]
- Felip E, Rosell R, Maestre JA, et al. Preoperative chemotherapy plus surgery versus surgery plus adjuvant chemotherapy versus surgery alone in early-stage non-small-cell lung cancer. J Clin Oncol 2010;28:3138-45. [PubMed]
- Pisters KM, Vallières E, Crowley JJ, et al. Surgery with or without preoperative paclitaxel and carboplatin in early-stage non-small-cell lung cancer: Southwest Oncology Group Trial S9900, an intergroup, randomized, phase III trial. J Clin Oncol 2010;28:1843-9. [PubMed]
- Scagliotti GV, Pastorino U, Vansteenkiste JF, et al. Randomized phase III study of surgery alone or surgery plus preoperative cisplatin and gemcitabine in stages IB to IIIA non-small-cell lung cancer. J Clin Oncol 2011;30:172-8. [PubMed]
- Betticher DC, Hsu Schmitz SF, Tötsch M, et al. Mediastinal lymph node clearance after docetaxel-cisplatin neoadjuvant chemotherapy is prognostic of survival in patients with stage IIIA pN2 non-small-cell lung cancer: a multicenter phase II trial. J Clin Oncol 2003;21:1752-9. [PubMed]
- Betticher DC, Hsu Schmitz SF, Tötsch M, et al. Prognostic factors affecting long-term in patients with resected stage IIIA pN2 non-small-cell lung cancer: 5-year follow-up of a phase II study. Br J Cancer 2006;94:1099-106. [PubMed]
- Machtay M, Lee JH, Stevenson JP, et al. Two commonly used neoadjuvant chemoradiotherapy regimens for locally advanced stage III non-small cell lung carcinoma: long-term results and associations with patholgic response. J Thorac Cardiovasc Surg 2004;127:108-13. [PubMed]
- Stamatis G, Eberhardt W, Pöttgen C. Surgery after multimodality treatment for non-small-cell lung cancer. Lung Cancer 2004;45 Suppl 2:S107-12. [PubMed]
- Pezzetta E, Stupp R, Zouhair A, et al. Comparison of neoadjuvant cisplatin-based chemotherapy versus radiochemotherapy followed by resection for stage III (N2) NSCLC. Eur J Cardiothorac Surg 2005;27:1092-8. [PubMed]
- Higgins K, Chino JP, Marks LB, et al. Preoperative chemotherapy versus preoperative chemoradiotherapy for stage III (N2) non-small-cell lung cancer. Int J Radiat Oncol Biol Phys 2009;75:1462-7. [PubMed]
- Kim AW, Liptay MJ, Bonomi P, et al. Neoadjuvant chemoradiation for clinically advanced non-small-cell lung cacner: an analysis of 233 patients. Ann Thorac Surg 2011;92:233-41; discussion 241-3. [PubMed]
- Paul S, Mirza F, Port JL, et al. Survival of patients with clinical stage IIIA non-small-cell lung cancer after induction therapy: age, mediastinal downstaging, and extent of pulmonary resection as independant predictors. J Thorac Cardiovasc Surg 2011;141:48-58. [PubMed]
- Shumway D, Corbin K, Salgia R, et al. Pathologic response rates following definitve dose image-guided chemoradiotherapy and resection for locally advanced non-small-cell lung cancer. Lung Cancer 2011;74:446-50. [PubMed]
- Pöttgen C, Eberhardt W, Graupner B, et al. Accelerated hyperfractionated radiotherapy within trimodality therapy concepts for stage IIIA/B non-small-cell lung cancer: Markedly higher rates of pathologic complete remissions than with conventional fractionation. Eur J Cancer 2013;49:2107-15. [PubMed]
- Koshy M, Fedewa SA, Malik R, et al. Improved survival associated with neoadjuvant chemoradiation in patients with clinical stage IIIA(N2) non-small-cell lung cancer. J Thorac Oncol 2013;8:915-22. [PubMed]
- Sher DJ, Fidler MJ, Liptay MJ, et al. Comparative effectiveness of neoadjuvant chemoradiotherapy versus chemotherapy alone followed by surgery for patients with stage IIIA non-small cell lung cancer. Lung Cancer 2015;88:267-74. [PubMed]
- Albain KS, Rusch V, Crowley JJ, et al. Concurrent cisplatin/etoposide plus chest radiotherapy followed by surgery for stages IIIA (N2) and IIIB non-small-cell lung cancer: mature results of Southwest Oncology Group phase II study 8805. J Clin Oncol 1995;13:1880-92. [PubMed]
- Ichinose Y, Fukuyama Y, Asoh H, et al. Induction chemoradiotherapy and surgical resection for selected stage IIIB non-small-cell lung cancer. Ann Thorac Surg 2003;76:1810-4; discussion 1815.
- Edelman MJ, Suntharalingam M, Burrows W, et al. Phase I/II trial of hyperfractionated radiation and chemotherapy followed by surgery in stage III lung cancer. Ann Thorac Surg 2008;86:903-10. [PubMed]
- D’Angelillo RM, Trodella L, Ciresa M, et al. Multimodality treatment of stage III non-small cell lung cancer: analysis of a phase II trial using preoperative cisplatin and gemcitabine with concurrent radiotherapy. J Thorac Oncol 2009;4:1517-23. [PubMed]
- Stupp R, Mayer M, Kann R, et al. Neoadjuvant chemotherapy and radiotherapy followed by surgery in selected patients with stage IIIB non-small-cell lung cancer: a multicentre phase II trial. Lancet Oncol 2009;10:785-93. [PubMed]
- Friedel G, Budach W, Dippon J, et al. Phase II trial of a trimodality regimen for stage III non-small-cell lung cancer using chemotherapy as induction treatment with concurrent hyperfractionated chemoradiation with carboplatin and paclitaxel followed by subsequent resection: a single-center study. J Clin Oncol 2010;28:942-8. [PubMed]
- Eberhardt WE, Gauler TC, Lepechoux C, et al. 10-year long-term survival (LTS) of induction chemotherapy with three cycles cisplatin/paclitaxel followed by concurrent chemoradiation cisplatin/etoposide/45 Gy (1.5 Gy bid) plus surgery in locally advanced non-small-cell lung cancer (NSCLC)-a multicenter phase-II trial (CISTAXOL). Lung Cancer 2013;82:83-9. [PubMed]
- Thomas M, Rübe C, Hoffknecht P, et al. Effect of preoperative chemoradiation in addition to preoperative chemotherapy: a randomised trial in stage III non-small-cell lung cancer. Lancet Oncol 2008;9:636-48. [PubMed]
- Girard N, Mornex F, Douillard JY, et al. Is neoadjuvant chemoradiotherapy a feasible strategy for stage IIIA-N2 non-small cell lung cancer? Mature results of the randomized IFCT-0101 phase II trial. Lung Cancer 2010;69:86-93. [PubMed]
- Katakami N, Tada H, Mitsudomi T, et al. A phase 3 study of induction treatment with concurrent chemoradiotherapy versus chemotherapy before surgery in patients with pathologically confirmed N2 stage IIIA nonsmall cell lung cancer (WJTOG9903). Cancer 2012;118:6126-35. [PubMed]
- Pless M, Stupp R, Ris HB, et al. Induction chemoradiation in stage IIIA/N2 non-small-cell lung cancer: a phase 3 randomised trial. Lancet 2015;386:1049-56. [PubMed]
- Aupérin A, Le Péchoux C, Rolland E, et al. Meta-analysis of concomitant versus sequential radiochemotherapy in locally advanced non-small-cell lung cancer. J Clin Oncol 2010;28:2181-90. [PubMed]
- van Meerbeeck JP, Kramer GW, Van Schil PE, et al. Randomized controlled trial of resection versus radiotherapy after induction chemotherapy in stage IIIA-N2 non-small-cell lung cancer. J Natl Cancer Inst 2007;99:442-50. [PubMed]
- Albain KS, Swann RS, Rusch VW, et al. Radiotherapy plus chemotherapy with or without surgical resection for stage III non-small-cell lung cancer: a phase III randomised controlled trial. Lancet 2009;374:379-86. [PubMed]
- Eberhardt WE, Pöttgen C, Gauler TC, et al. Phase III Study of Surgery Versus Definitive Concurrent Chemoradiotherapy Boost in Patients With Resectable Stage IIIA(N2) and Selected IIIB Non-Small-Cell Lung Cancer After Induction Chemotherapy and Concurrent Chemoradiotherapy (ESPATUE). J Clin Oncol 2015;33:4194-201. [PubMed]
- Rusch VW, Giroux DJ, Kraut MJ, et al. Induction chemoradiation and surgical resection for superior sulcus non-small-cell lung carcinomas: long-term results of Southwest Oncology Group Trial 9416 (Intergroup Trial 0160). J Clin Oncol 2007;25:313-8. [PubMed]
- Kunitoh H, Kato H, Tsuboi M, et al. Phase II trial of preoperative chemoradiotherapy followed by surgical resection in patients with superior sulcus non-small-cell lung cancers: report of Japan Clinical Oncology Group trial 9806. J Clin Oncol 2008;26:644-9. [PubMed]